Will Medicaid Pay for Assisted Living?

Introduction - What Is Assisted Living?
Assisted living is a type of long-term care that provides support and assistance with activities of daily living (ADLs), such as bathing, dressing, and managing medications. It is designed to help those who need more help than can be provided in a traditional independent living facility, but do not require the 24-hour medical attention of a nursing home.
Assisted living facilities are usually located in residential communities with on-site staff and amenities. These typically include meals, housekeeping, laundry services, transportation, and recreational activities. Residents have their own private apartments or rooms and can receive personalized care tailored to their needs.
Assisted living is known for its emphasis on maintaining independence and dignity. The staff provides assistance and support to help residents enjoy a high quality of life, while also ensuring safety and security. In addition, many facilities offer access to physical, occupational, and speech therapy.
The cost of assisted living varies depending on location, amenities, and level of care needed. In some cases, Medicare and Medicaid may help cover the cost of care. This guide will provide an overview of what Medicaid covers for assisted living and what families should consider when evaluating their options.
What Is Medicaid and How Does It Work?
Medicaid is a health insurance program funded by the federal government and administered by individual states. The program provides health care coverage to individuals and families who meet certain criteria regarding their income, disability, and other qualifications. Medicaid can cover a variety of medical expenses, from doctor's visits and hospitalizations, to preventive and long-term care services.
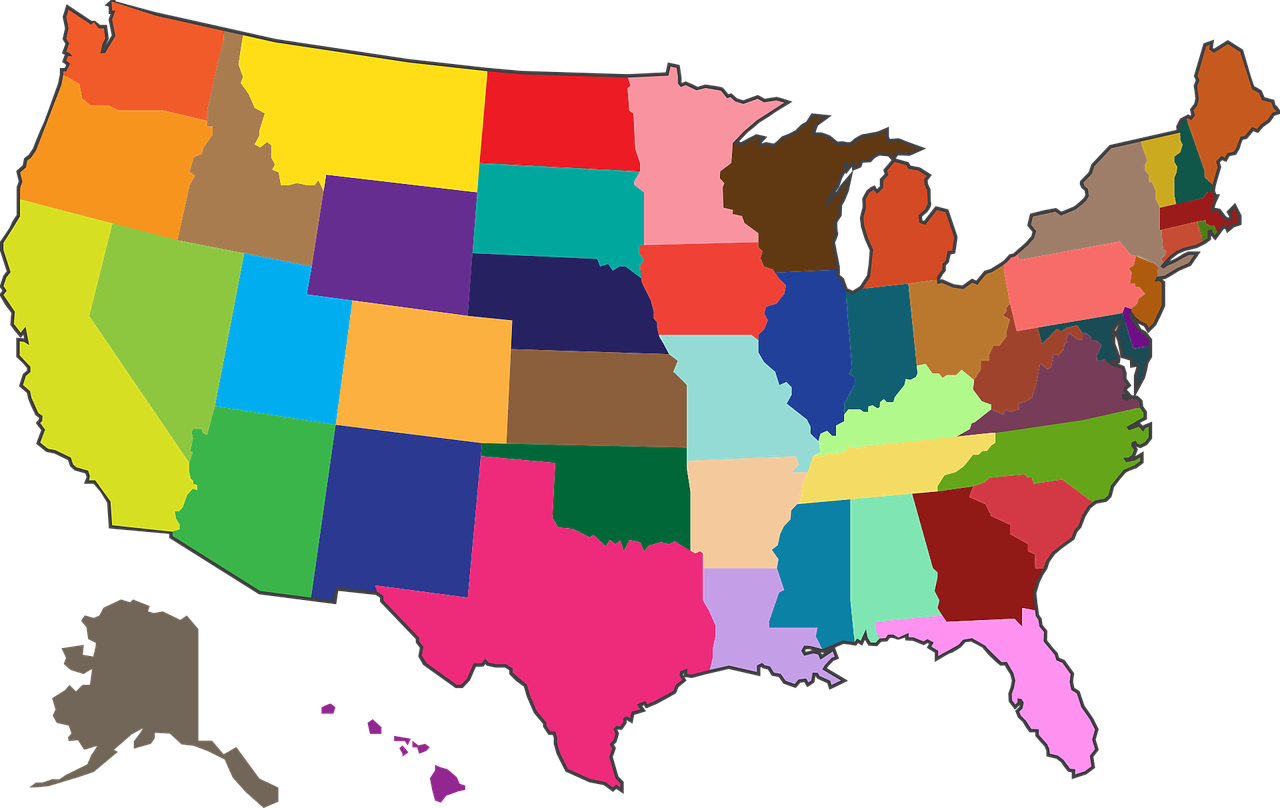
When it comes to assisted living, Medicaid can provide varying levels of coverage depending on the state you live in. Generally speaking, most states offer Medicaid-funded assisted living care for individuals who meet specific eligibility requirements.
There are two main types of Medicaid programs that cover assisted living: Community Medicaid and Home and Community-Based Services (HCBS). State Medicaid programs may provide coverage for both types, though Community Medicaid is more widely available.
Community Medicaid is a Medicaid program specifically for elderly and disabled individuals who need long-term services and support. In order to be eligible for this program, individuals must meet certain financial criteria and must use their Medicaid benefits to pay for costs associated with assisted living.
In contrast, Home and Community-Based Services (HCBS) is a type of Medicaid program that provides coverage for individuals who need home care and other community-based services. HCBS covers services such as personal care attendant services, daycare, and transportation.
Both Community Medicaid and HCBS allow eligible individuals to have more control over where they receive care and who provides it. In addition, both programs offer benefits that are not available through traditional Medicaid programs, such as private pay options and flexible spending accounts.
Despite these benefits, there are some downsides to Medicaid assisted living coverage. For example, many states have very strict eligibility requirements and it can be difficult for individuals to qualify. Additionally, Medicaid reimbursement rates for assisted living facilities are often lower than those for nursing homes, making it harder for facilities to provide quality care.
Nevertheless, Medicaid is an important resource for those looking for help with the costs of assisted living care. With the right information, individuals and families can make informed decisions about what type of care is best for them.
What Types of Care Does Medicaid Cover for Assisted Living?
Assisted living is a type of care that provides elderly individuals with assistance in their everyday activities. At an assisted living facility, residents are provided all of the necessary services and supplies needed to live comfortably, including meals, housekeeping, medical care, and various social activities. Assisted living facilities may also provide additional services such as transportation, recreational outings, and therapy.
Medicaid is a program designed to provide health insurance to low-income individuals and families. Depending on the state in which you live, Medicaid may cover some or all of the costs associated with living in an assisted living facility. However, it is important to note that Medicaid coverage varies from state to state, so it is best to check with your state's Medicaid website or call your local Medicaid office to see what types of care it covers.
In general, Medicaid will usually cover the cost of room and board at an assisted living facility, as well as personal care services such as help with dressing, bathing, and eating. It may also cover additional services such as medication management, physical therapy, and home health care services. In some cases, it may even cover the cost of medical supplies and equipment related to nursing care.
It is important to keep in mind that Medicaid may not cover all of the services offered by an assisted living facility. It is always best to check with your state's Medicaid office or your local assisted living facility to make sure that the services you need are covered.
Eligibility Requirements for Medicaid Assisted Living Benefits
Medicaid is a federal health care program that covers the cost of medical care for those in financial need. It is administered by the states, but all programs must adhere to the guidelines set forth by the federal government. Each state has different eligibility requirements, but there are a few general points to consider when seeking Medicaid coverage for assisted living.
The first step in determining eligibility for Medicaid coverage is to determine your income level. Medicaid is an income-based program, meaning that it is available only to those who are below certain income levels. The exact income levels vary from state to state, so it's important to check with your local Medicaid office or health care provider for the details. Generally, you must have an income less than twice the poverty line to qualify.
Other factors that may affect your eligibility include your living situation, whether you receive other forms of public assistance, and whether you need long-term or short-term care. Generally, if you are over the age of 65, disabled, or blind, and have limited assets, you are more likely to qualify for Medicaid coverage. You may also be eligible if you are pregnant, have a child under the age of 21, or are a veteran.
It is important to note that Medicaid does not automatically cover all assisted living costs. Depending on your individual situation, some services or living arrangements may not be covered. For example, semi-private rooms, room and board, or private care services may not be covered by Medicaid. Additionally, Medicaid does not typically cover the cost of recreational activities, such as golf, swimming, or movies. It is best to contact your local Medicaid office to discuss what types of services are covered.
When it comes to covering the costs of assisted living, Medicaid can be a valuable resource for those who meet the eligibility requirements. Medicaid is a U.S. federal and state health insurance program for people with low incomes and limited resources. This guide will explain how to determine if you are eligible for Medicaid coverage for assisted living and how to navigate the application process.
To qualify for Medicaid coverage for assisted living, you must meet specific financial and medical criteria. Generally, you must be 65 years old or older, blind, disabled, or enrolled in Medicare. Additionally, applicants must have limited income and assets to be approved for Medicaid assisted living benefits.
Income limits vary based on your state, but are typically set at or below 100 percent of the Federal Poverty Limit (FPL). Assets are calculated differently for those who are qpplying for nursing home care, and those who are applying for assistance with living in their own home or an assisted living facility. In most cases, your home, one car, and some other personal property won’t count toward your asset limit, but other things such as bank accounts, stocks, bonds, and cash do. To get an exact assessment of your eligibility, contact your local Medicaid office.
In order to be approved for Medicaid coverage for assisted living, applicants must also demonstrate a need for additional care. A medical evaluation must be completed by a doctor or other medical professional to determine if a person has long-term care needs such as help with activities of daily living (ADLs) such as bathing, dressing, or eating.
Once the eligibility process is complete, Medicaid will cover the costs of assisted living services such as room and board, meals, medication management, recreational activities, and more. In some states, Medicaid may also provide extra services such as physical and occupational therapy, as well as transportation assistance.
Before submitting your Medicaid application, make sure you have all the necessary documentation and information ready. You will need to provide proof of identity, including a driver's license or Social Security card, as well as proof of residence and proof of income. You will also need to provide a detailed list of your assets and any financial records or statements showing the value of your property. If you are married, you may need additional documentation from your spouse.
It is important to remember that Medicaid is a means-tested program. This means applicants must demonstrate financial hardship to qualify for assistance. If your income and assets exceed the limits set by your state’s Medicaid program, you may not be eligible for coverage.
By understanding the Medicaid eligibility requirements and the types of care covered by the program, you can make an informed decision about whether Medicaid assisted living is right for you or your loved one.
Documentation Needed for Assisted Living Medicaid Benefits
Before qualifying for Medicaid assisted living benefits, you must provide a variety of documentation. This includes income and asset statements, as well as proof of residency, age, and health status.
When applying for Medicaid coverage, you will need to provide proof of your assets and income with reports such as pay stubs, bank statements, Social Security benefit statements, pension statements, and more. These documents will help the Medicaid representative determine your eligibility for assisted living benefits.
Generally, Medicaid applicants are also required to provide proof of their age and residency. You may be asked to submit a birth certificate, driver’s license, or any other type of identification that proves residency in the state where you are applying for benefits. You may also need to submit medical documentation related to your overall health status.
Keep in mind that the documentation requirements can vary from state to state. Your Medicaid representative will provide you with detailed information about the type of documentation needed in order to qualify.
Programs That Offer Financial Assistance for Assisted Living Costs
When facing the cost of assisted living, finding financial assistance is essential. Medicaid is the largest source of funding for financially-needy seniors to cover the costs of long-term care services such as assisted living. However, there are other programs available that may supplement or act as a substitute for Medicaid.
For those who require additional financial assistance, there are a few government and private programs to look into. State, local, and tribal governments offer different programs depending on the state you reside in. These programs provide assistance to seniors with low incomes and limited resources.
One of the more popular programs is the Program of All-Inclusive Care for the Elderly (PACE). Developed through a partnership between Medicare and Medicaid, PACE focuses on providing community-based health care and social services to eligible adults aged 55 and over. This program offers a comprehensive health plan for medical and social services, including meals and assisted living. PACE also focuses on helping seniors age in place instead of nursing homes, and can help reduce the cost of long-term care services.
Other programs include the Veterans Aid & Attendance Pension, the Supplemental Security Income (SSI), and reverse mortgage loans. The Veterans Aid & Attendance Pension is a benefit for veterans 65 or older, surviving spouses, and disabled veterans. Those enrolled in the program may be eligible for cash assistance to help cover the cost of assisted living. The SSI program provides financial assistance to aged, blind, or disabled people who have limited income and resources. As for reverse mortgage loans, these are loans that allow homeowners to access their home’s equity and receive payments from the lender.
These are just some of the potential programs available to assist with the cost of assisted living. It’s important to research what types of assistance are available in your state since the programs vary from state to state.
Benefits and Drawbacks of Medicaid Assisted Living Coverage
Medicaid provides an important resource to many families who cannot otherwise afford the costs associated with assisted living. For those who qualify, the coverage offers a range of benefits, though there are also drawbacks to consider.
Benefits of Medicaid Assisted Living Coverage
The primary benefit of Medicaid coverage for assisted living is its affordability. Without this coverage, the costs of assisted living can be prohibitively expensive, making it inaccessible to many families. Medicaid may also cover certain additional services, such as medical care and physical therapy, that are not offered in other types of living arrangements. Furthermore, Medicaid eligibility grants access to a broad network of healthcare providers, giving families access to experienced professionals.
Drawbacks of Medicaid Assisted Living Coverage
Though Medicaid assisted living coverage is often a financial lifeline, there are some drawbacks to consider. Many states have strict eligibility requirements that limit who can qualify for benefits. Furthermore, even among qualified residents, coverage may be limited to a certain number of days or services. Additionally, not all assisted living facilities accept Medicaid, so families may have a limited selection of facilities to choose from. Lastly, since Medicaid coverage is often times tied to the state where a person resides, individuals may not qualify for Medicaid coverage if they move out of state.
In conclusion, the decision to pursue Medicaid assistance for assisted living should be made carefully. The coverage offers financial assistance and expanded access to healthcare providers, but it also has some drawbacks. Families should weigh the costs and benefits of Medicaid coverage when deciding whether it is right for them.
Navigating the Application and Approval Process
Applying for Medicaid to help pay for assisted living expenses can be a difficult and time-consuming process. But, with a little bit of effort, you can successfully navigate the application and approval process.
The most important thing to remember is that each state has different eligibility requirements and processes for applying for Medicaid benefits. It's important to research your state's guidelines thoroughly. You can find this information through your state's Department of Health and Human Services website.
If you decide to apply for Medicaid to cover some or all of your assisted living expenses, you'll need to provide proof of residency, income, assets, medical expenses, and other information.
Once you have gathered all of the necessary documents, you'll need to fill out an application form. This will ask for detailed information about yourself and your financial situation. Once you have completed the form, you'll need to submit it to your state's Medicaid office.
After submitting the application, you'll receive a letter from the Medicaid office informing you if you have been approved or denied for coverage. Keep in mind that it can take several weeks or months for the application to be processed.
If your application is denied, you may be able to appeal the decision by filing an appeal with your state’s Medicaid office. You may also want to consult with a lawyer or other legal professional to help you understand how to best handle the appeal process.
Finally, once you have been approved for Medicaid coverage, you'll need to contact your assisted living facility to ensure that they are able to accept Medicaid payments. Be sure to double-check all of the relevant details before signing any contracts.
Questions Families Should Ask When Considering Assisted Living Facilities Covered by Medicaid
When selecting an assisted living facility for a loved one, it is essential to ask the right questions to ensure that the facility is able to meet the individual's specific needs. Aside from researching if the facility qualifies for Medicaid coverage, families should also consider the following questions when selecting a facility for a family member or friend:
- What types of services are offered? Is there on-site medical care, meals, activities, and housekeeping services?
- What is the ratio of staff to residents?
- How spacious is the living area? Are there shared rooms or private bedrooms and bathrooms?
- Are there any additional fees or special charges for specific treatments or services?
- What safety features are in place? Are there alarms or other protective measures?
- What is included in the monthly rent?
- What happens if the resident's health declines and they need more care than the facility can provide?
Asking these questions helps families gain insight into what day-to-day life will be like for their loved one in the selected assisted living facility. It also reduces the chance of being surprised by any unexpected costs or policies associated with the facility. Knowing the answers to these questions can provide peace of mind that the facility is the right fit for the individual's long-term needs.
Commonly Asked Questions about Medicaid Assisted Living Coverage
When it comes to using Medicaid to cover assisted living costs, there are several important questions to consider. To help you choose the best assisted living option for your loved one, here are some of the most common questions people have about Medicaid and assisted living.
Can I get Medicaid to pay for assisted living?
In most cases, yes. Medicaid may cover some or all of the cost of assisted living, depending on your loved one's eligibility and the guidelines of the state they live in. It is important to check with your local Medicaid office to see which services are covered.
Will Medicaid cover all of my assisted living costs?
No, Medicaid will not cover all of the costs of assisted living. Typically, Medicaid will only cover a portion of the cost. To determine exactly how much Medicaid will cover, you need to contact your local Medicaid office.
What other financial assistance programs are available for assisted living costs?
There are several other programs that can help cover the cost of assisted living. For example, veterans may be eligible for aid and attendance benefits which can be used for assisted living expenses. Additionally, many states offer waivers to cover the cost of long-term care, including assisted living. You should speak to your local Medicaid office or veterans’ benefits office to find out more about available options.
What documents do I need to apply for Medicaid coverage?
When you apply for Medicaid assistance, you will need to provide proof of your income, assets, and expenses. Additionally, you may need to provide medical records and proof of U.S. citizenship or legal residency. Check with your local Medicaid office for more information about the specific documents required.
Conclusion – Are Assisted Living and Medicaid a Good Fit?
So, is Medicaid the right choice for you or your loved one’s assisted living needs? Medicaid programs can help those who are low-income and meet certain eligibility requirements cover some of the costs associated with living in a nursing home or assisted living facility. However, it’s important to realize that there are both benefits and drawbacks to using Medicaid to pay for these medical services. It’s important to consider your family’s financial situation as well as the individual’s medical care needs when determining if Medicaid is the right fit.
It’s also important to remember that it is possible to qualify for Medicaid even if you have some assets. As long as you meet the eligibility requirements, you may still be able to use Medicaid to pay for assisted living. However, it’s always best to discuss your situation with a qualified Medicaid specialist before making any decisions.
You might also like this article: