What is Binswanger's Disease? Subcortical Dementia Syndrome
Subcortical Dementia Syndrome (Binswanger's Disease) is a type of dementia that affects the subcortical areas of the brain, causing symptoms such as tremors, memory difficulties, and emotional instability.

Discover Binswanger's Disease: A Guide to Understanding and Managing Subcortical Vascular Dementia
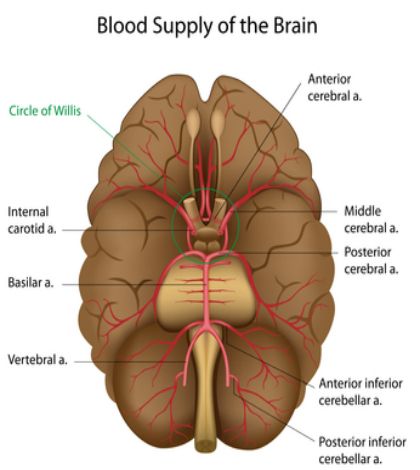
What if there was a type of dementia that involves microscopic damage to the brain's white matter, leading to cognitive impairment and behavioral changes? Look no further than Binswanger's disease, also known as subcortical vascular dementia. This condition is caused by the thickening and narrowing of arteries, resulting in decreased blood flow and the death of brain tissue.
But don't lose hope—there are ways to improve care for those affected by Binswanger's disease. Consider participating in a clinical trial, where medical professionals and scientists are working hard to learn more about this disorder and find better ways to detect, treat, and prevent it. Volunteers of all ages, backgrounds, and health statuses are needed to ensure that the study results can benefit as many people as possible.
Although there is no specific treatment for Binswanger's disease, there are symptomatic approaches that can help manage its effects. Antidepressant and antipsychotic medications may be prescribed to address depression, anxiety, and agitation. Additionally, recent drug trials have shown promising results in improving cognition and stabilizing overall functioning and behavior.
To slow the progression of Binswanger's disease, it is crucial to prioritize prevention. Managing hypertension, diabetes, and other risk factors through a healthy lifestyle—proper diet, exercise, and avoiding smoking and excessive alcohol consumption—can make a significant difference.
While Binswanger's disease is a progressive condition with no cure, there is ongoing research dedicated to finding better solutions. Organizations like the National Institute of Neurological Disorders and Stroke are actively investigating ways to prevent, treat, and ultimately cure neurological disorders, including Binswanger's disease.
Join the fight against Binswanger's disease. Together, we can make a difference by understanding, managing, and researching this complex condition.
Symptoms of Binswanger's Disease
Doctors see symptoms of subcortical dementia syndrome more often in patients with Huntington’s or Parkinson’s disease rather than Alzheimer’s Disease because of where damage occurs. The sub-cortical area of the brain contains structures controlling personality, movement, and mood–the cerebellum, the basal ganglia and the brain-stem nuclei.
Sometimes called the “little brain”, the cerebellum is primarily concerned with human motor control. When damage occurs to this portion of the brain, coordination, balance and the ability to perform skilled, precise movements is impaired.
The cerebellum also assists cortical structures with fine-tuning attention and learning abilities, especially when learning something new involves assessing sensory input and planning motility actions.
Consisting of five different nuclei that includes the nucleus accumbens, substantia nigra, and caudate nucleus, the basal ganglia are responsible for receiving vast amounts of information from the cerebral cortex, processing this information and then transmitting it back to the cortex through the thalamus.
When Binswanger's disease, subcortical dementia syndrome symptoms affect an individual with Parkinson’s or Alzheimer’s, it is this cortico-basal ganglia-cortical loop that is disrupted enough to cause symptoms such as:
- Tremors and muscle spasms
- Memory difficulties
- Inability to recall everyday words
- Slowed or involuntary movements
- Emotional instability
The brainstem nuclei, or simply the brainstem, is the evolutionarily oldest part of the brain and connects the spinal cord to the cerebrum. Sensory and motor neurons pass through the brainstem up into the brain where information is received and processed by various parts of the brain.
Without the brainstem, humans would not be able to perform automatic functions such as breathing, regulation of blood pressure and heart rate and food digestion. In regards to subcortical dementia symptoms, an affected brain stem will produce deficits in alertness and arousal, speech and visual problems and muscle weakness.
Personality and Mood Changes
Apathy, depression, disinhibition (socially inappropriate behavior), and irritability represent the primary changes in mood and personality caused by this type of dementia. Alternately, individuals with specific, cortical-type dementia will suffer more severe issues with language, memory and problem-solving than with mood. However, these dementias sometimes co-exist, especially in advanced stages of Alzheimer’s or vascular dementia and eventually present other classic symptoms associated with Alzheimer’s disease.
Medical conditions causing the onset and development of subcortical dementia include:
- Chronic alcoholism
- Vascular dementia
- Late-stage Parkinson’s disease
- AIDS dementia complex
- Lyme disease
- Brain tumors
- Huntington’s and Wilson’s disease
- Multiple sclerosis
- Severe head traumas
Effective Treatment for BD: Managing Symptoms and Slowing Progress
When it comes to treating BD, there is no one-size-fits-all solution. Treatment focuses on alleviating symptoms, and for individuals with depression or anxiety, antidepressant medications such as sertraline or citalopram can be beneficial. Atypical antipsychotic drugs like risperidone and olanzapine are useful for managing agitation and disruptive behavior. Excitingly, recent drug trials with memantine have shown improved cognition and stabilization of overall functioning and behavior.
Beyond medication, effectively managing hypertension and diabetes can slow the progression of atherosclerosis, subsequently slowing the progress of BD. While there is no cure for the disease, taking preventive measures early in adulthood, such as controlling risk factors like hypertension, diabetes, and smoking, can greatly improve outcomes.
Prognosis: Understanding the Progressive Nature of BD
BD is a progressive disease with no cure. Changes can occur suddenly or gradually, progressing in a stepwise manner. It's important to note that BD can often coexist with Alzheimer's disease. However, adopting healthy lifestyle behaviors, such as eating a nutritious diet, maintaining regular sleep patterns, exercising, and avoiding excessive smoking or alcohol consumption, can also slow down the progression of BD.
Advancing Research Towards Prevention, Treatment, and Cure
The National Institute of Neurological Disorders and Stroke (NINDS) leads extensive research on BD in their laboratories at the National Institutes of Health (NIH). They also provide grants to major medical institutions nationwide, fueling additional research to uncover better ways to prevent, treat, and ultimately cure neurological disorders like BD. Exciting developments lie ahead!
Obtaining an accurate diagnosis regarding the cause of subcortical dementia symptoms is vital to receiving appropriate and effective treatment. Complete physical, neurological and neuropsychological testing is necessary before medications can be prescribed. Cognitive abilities are usually assessed by giving patients the Mini-Mental State Examination. Brain imaging scans will also provide information about the condition of the brain and reveal areas that are experiencing signs of degeneration.
Individuals suffering from moderate to severe AD exhibit abnormal electroencephalo-grams when subjected to EEG tests. Patients with Parkinson’s or Huntington’s reveal contrasting electrical brain wave patterns from those with AD, enabling physicians to give a more accurate diagnosis when confronted with a dementia patient.
Lab tests used to rule out other medical conditions and contribute to a precise diagnosis of dementia include blood glucose, complete blood count, thyroid, urinalysis, and cerebrospinal fluid screening.

Patients suspected of suffering from Parkinson’s rather than Alzheimer’s are given a drug called levodopa, or L-dopa. Because Parkinson’s disease results from reduced dopamine levels in the brain, L-dopa (a precursor to dopamine) is provided to see if motor impairment is alleviated. If the jerkiness, tremors, stiffness and involuntary movements associated with Parkinson’s is not relieved, then doctors may rule out Parkinson’s and continue treatment plans beneficial to a diagnosis of vascular dementia or Alzheimer’s disease upon completion of further testing.
Unless dementia is caused by a reversible condition such as operable tumors, metabolic syndromes, or nutritional deficiencies, it remains incurable. Attempting to control symptoms and keep patients as comfortable as possible is currently the best treatment method.
Patients suffering subcortical as well as cortical dementias will need pervasive, if not 24 hour care, in advanced stages of the disease. Drugs such as atypical neuroleptics (Risperdal or Depakote) and antidepressants (Paxil or Effexor) may help reduce the irritability, disinhibition, motor difficulties, and depression associated with this type of dementia.
Preventing Dementia
Although research has yet to discover why Parkinson’s and Huntington’s disease is triggered in certain individuals, belief that a genetic component may exist to explain the origin of the disease is a theory popular among neurologists.
However, it is possible to prevent or substantially delay the development and progression of Binswanger's disease due to Alzheimer’s disease or vascular dementia by adopting a lifestyle that emphasizes regular exercise, a healthy diet, avoidance of smoking, excessive alcohol intake and chronic stress. In addition, engaging in intellectual stimulation promotes the ability of the brain to grow new connections among neurons, an action that has been proved in research to effectively avert the development of Alzheimer’s disease.
Get your free Dementia Prevention Report here
Discover the Causes and Symptoms of Binswanger Disease and Take Control of Your Health
Binswanger disease, a form of vascular dementia, is caused by various factors including arteriosclerosis, thromboembolism, and other conditions that restrict blood flow to the brain. Major risk factors include hypertension, hypercholesterolemia, cardiac disease, sleep apnea, atrial fibrillation, diabetes mellitus, and smoking. It can also be caused by rare genetic diseases like CADASIL.
What sets Binswanger disease apart is its clinical progression, with cognitive impairment and neurological symptoms gradually worsening over time. Typically appearing between the ages of 50 and 70, Binswanger disease can last from five to ten years. This condition is characterized by dementia and a dysexecutive syndrome, leading to cognitive and behavioral abnormalities.
People affected by Binswanger disease often experience inactivity, apathy, depression, and a lack of decision-making ability. They may exhibit poor judgment, difficulty with planning and organization, and decreased communication. Other symptoms can include trouble speaking, swallowing, and controlling the bladder.
Some patients with Binswanger disease may also show signs of Parkinsonism, with slowness, poor balance, and shuffling steps. It is important to note that tremor is not a common symptom. Many individuals with Binswanger disease have also experienced strokes or transient ischemic episodes in the past.
There can be a co-existence of Binswanger disease with Alzheimer's disease, as both conditions become more prevalent with age.
To diagnose Binswanger disease, a thorough clinical evaluation including patient history, physical examination, and brain imaging such as MRI or CT scans is commonly used. Treatment focuses on managing stroke risk factors to slow the disease's progression. This can include medications to control blood pressure, prevent thromboembolism and atherosclerosis, as well as addressing other underlying conditions like depression and diabetes.
Physical therapy and exercise programs can help improve balance and manage parkinsonian symptoms. In addition, certain medications like risperidone and olanzapine may be prescribed for agitation and disruptive behavior.
While there is no cure for Binswanger disease, early intervention and management of risk factors such as hypertension, diabetes, and smoking can make a significant difference in controlling its advancement.
Take charge of your health and empower yourself with knowledge about Binswanger disease.
http://www.nlm.nih.gov/medlineplus/ency/article/001069.htm
http://www.biology.emory.edu/research/Jaeger/BasalGanglia/BG_page.html
Our Resource section can help you find the information and tools that you need. We have courses, videos, checklists, guidebooks, cheat sheets, how-to guides and more.
You can get started by clicking on the link below. We know that taking care of a loved one is hard work, but with our help you can get the support that you need.
Click here to go to Resource Section now!
You might also like this article:







