Understanding Vascular Dementia: Causes, Symptoms, and Management Strategies
Explore the complexities of vascular dementia, including its causes, symptoms, and management strategies. Learn about its relationship with Alzheimer's, the importance of blood flow and vessel health, and the crucial role of managing risk factors in preventing

Vascular dementia is a complex and challenging condition that affects millions worldwide. Understanding its causes, symptoms, and management is crucial for patients, their families, and healthcare professionals. This article delves into the intricacies of vascular dementia, exploring its relationship with Alzheimer's disease, risk factors, diagnostic processes, and management strategies.
What is Vascular Dementia?
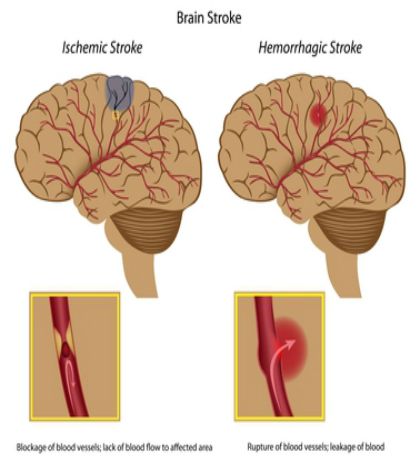
Vascular dementia occurs when the brain's blood supply is disrupted, leading to damaged brain cells. This condition often results from blood vessel blockages or damage, leading to strokes or bleeding in the brain. It can occur on its own or alongside Alzheimer's disease, forming a condition known as mixed dementia.
Vascular dementia is a neurological disorder caused by impaired blood flow to the brain. This disruption, often resulting from blood vessel blockages or damage, leads to the death of brain cells. The condition is typically associated with stroke or transient ischemic attacks (TIAs), where the blood supply to certain parts of the brain is temporarily reduced. Additionally, small vessel disease, which affects the brain's smaller blood vessels, can contribute to the development of vascular dementia.
Relationship with Alzheimer's Disease
Exploring the Relationship Between Vascular Dementia and Alzheimer's Disease
Vascular dementia and Alzheimer's disease are two prevalent forms of dementia that, despite sharing some similarities, have distinct causes and characteristics. Understanding their relationship is crucial for diagnosis, treatment, and management.
Vascular Dementia: A Focus on Blood Flow and Blood Vessels
Vascular dementia is primarily caused by reduced blood flow to the brain, leading to the death of brain cells. This reduction in blood flow can result from various factors, including:
Stroke and Transient Ischemic Attack (TIA): These events can block or reduce blood flow in the brain's blood vessels, causing damage.
Small Vessel Disease: This condition affects smaller blood vessels, leading to reduced blood supply and brain damage.
Heart Conditions: Atrial fibrillation and other heart diseases can lead to the formation of blood clots, disrupting blood flow to the brain.
Symptoms of vascular dementia often include difficulties with problem-solving, planning, and organizing, which are more pronounced than memory loss in the early stages.
Alzheimer's Disease: The Role of Brain Cellular Changes
In contrast, Alzheimer's disease is characterized by the accumulation of amyloid plaques and tau tangles in the brain. These abnormal protein deposits lead to the death of brain cells and the disruption of normal brain function. Alzheimer's typically presents with memory loss as one of the earliest symptoms, followed by other cognitive impairments.
Vascular dementia and Alzheimer's disease are two of the most common forms of dementia. While Alzheimer's is primarily related to the build-up of plaques and tangles in the brain, vascular dementia is caused by problems in blood flow. In many cases, patients may suffer from mixed dementia, which includes symptoms of both Alzheimer's and vascular dementia.
Symptoms and Progression
The symptoms of vascular dementia can vary but generally include:
- Cognitive Impairment: Difficulty with concentration, decision-making, and memory.
- Physical Symptoms: Stroke symptoms, such as physical weakness or paralysis.
- Mood Changes: Depression and apathy.
- Functional Decline: Difficulty in managing daily tasks.
The progression of vascular dementia can be gradual or occur in a series of steps, often corresponding to strokes or other vascular events.
The Link Between Blood Flow and Brain Health
The brain relies on a network of blood vessels to function correctly. Any disruption in blood flow can significantly impact brain function, leading to symptoms of dementia. Conditions like high blood pressure, atrial fibrillation, and other circulatory diseases can damage blood vessels, increasing the risk of vascular dementia.
Early Symptoms and Progression
Early symptoms of vascular dementia can include memory loss, confusion, and difficulty concentrating. These symptoms may gradually worsen or occur suddenly following a stroke. Unlike Alzheimer's, where symptoms typically develop slowly, vascular dementia can have a more abrupt onset due to its association with stroke-like events.
Risk Factors for Developing Vascular Dementia
Several factors increase the risk of developing vascular dementia. High blood pressure and high cholesterol are significant contributors, as they can lead to the narrowing and damage of brain blood vessels. Lifestyle factors like smoking, obesity, and physical inactivity also play a crucial role. Furthermore, conditions like heart disease, diabetes, and atrial fibrillation are linked with an increased risk.
Identifying and Managing Risk Factors for Vascular Dementia
Vascular dementia, a common form of dementia, often results from decreased blood flow to the brain, leading to damaged brain cells. Identifying and managing risk factors is essential in preventing or slowing the progression of vascular dementia. This approach also benefits those at risk of Alzheimer's disease and other cognitive impairments.

Understanding Risk Factors
Key risk factors for vascular dementia include:
High Blood Pressure: Chronic high blood pressure can damage blood vessels in the brain, impairing blood flow.
High Cholesterol: Elevated cholesterol levels can lead to the buildup of plaques in blood vessels, reducing blood supply to the brain.
Heart Disease: Conditions like atrial fibrillation can disrupt blood flow, increasing the risk of stroke and, consequently, vascular dementia.
Diabetes: Poorly managed diabetes increases the risk of vascular changes that can affect the brain.
Lifestyle Factors: Smoking, excessive alcohol intake, physical inactivity, and an unhealthy diet are significant contributors.
Strategies for Managing Risk Factors
Controlling Blood Pressure: Regular monitoring and medication, if necessary, can keep blood pressure within a healthy range, protecting brain blood vessels.
Managing Cholesterol Levels: A diet low in saturated fats, regular exercise, and cholesterol-lowering medications can help maintain healthy cholesterol levels.
Heart Health: Managing heart conditions, such as atrial fibrillation, with medication and lifestyle changes can reduce the risk of blood clots and stroke.
Lifestyle Modifications:
Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support vascular health.
Physical Activity: Regular exercise, such as walking, swimming, or cycling, helps maintain heart and blood vessel health.
Quitting Smoking: Smoking cessation is crucial as it directly damages blood vessels and increases the risk of stroke.
Moderating Alcohol Consumption: Limiting alcohol intake can reduce blood pressure and the risk of heart disease.
Role of Healthcare Professionals
Healthcare professionals play a critical role in identifying individuals at risk and guiding them in managing these risk factors. This includes regular health check-ups, monitoring for early symptoms of vascular dementia, and providing resources for lifestyle changes.

Importance of Family Support
Family members can support their loved ones by encouraging healthy lifestyle habits, assisting in managing medical conditions, and providing emotional support.
Monitoring Cognitive Health
Regular cognitive assessments can help detect early signs of cognitive decline, allowing for timely interventions. This is especially important in individuals with risk factors for vascular dementia or those experiencing early symptoms.
Research and Clinical Trials
Ongoing research and clinical trials are continually exploring new ways to prevent and treat vascular dementia. These studies focus on various aspects, including the efficacy of new medications, lifestyle interventions, and understanding the disease's pathology.
Effective management of risk factors for vascular dementia involves a combination of medical interventions, lifestyle changes, and support from healthcare professionals and family members. By addressing these risk factors, it is possible to significantly reduce the likelihood of developing vascular dementia, improve overall brain health, and maintain a higher quality of life.
Diagnosing Vascular Dementia
Diagnosing vascular dementia involves a comprehensive evaluation, including a full medical history, neurological exams, and brain imaging tests. These assessments help differentiate vascular dementia from Alzheimer's and other forms of dementia. Healthcare professionals look for evidence of stroke or small vessel disease, as well as signs of cognitive impairment and memory loss.
The Role of Brain Imaging
Brain imaging plays a crucial role in diagnosing vascular dementia. Techniques like MRI and CT scans can reveal changes in the brain's structure, such as evidence of stroke or blood vessel damage. These images help in assessing the extent of brain damage and in formulating an effective treatment plan.
Differentiating Vascular Dementia from Alzheimer's
While both vascular dementia and Alzheimer's disease affect memory and cognitive abilities, they have different causes and symptoms. Alzheimer's is primarily caused by the buildup of plaques and tangles in the brain, while vascular dementia results from reduced blood flow and oxygen to the brain. The progression of symptoms also tends to be different, with vascular dementia often presenting with a stepwise decline following each stroke or vascular event.

Mixed Dementia: A Combination of Vascular and Alzheimer's
In some cases, individuals may have mixed dementia, which includes features of both Alzheimer's and vascular dementia. This can complicate diagnosis and treatment, as symptoms and progression patterns may vary widely.
Treatment and Management of Vascular Dementia
While there is no cure for vascular dementia, treatment focuses on managing symptoms and slowing progression. This includes medications to control blood pressure, cholesterol, and prevent blood clots. Cognitive therapies and rehabilitation can also help improve brain function and quality of life.
Lifestyle Changes and Support
Lifestyle changes play a significant role in managing vascular dementia. Adopting a heart-healthy lifestyle, engaging in regular physical activity, and following a balanced diet can help manage risk factors. Support from family members and healthcare professionals is also crucial in providing care and managing daily challenges.
Research and Future Directions
Ongoing research and clinical trials are exploring new treatments and interventions for vascular dementia. This includes studying the impact of lifestyle factors, new medications, and therapies to improve brain function and slow disease progression.
The Importance of Early Intervention
Early intervention is key in managing vascular dementia. Recognizing symptoms early and addressing risk factors can significantly impact the disease's progression. Healthcare professionals play a crucial role in educating patients and their families about the importance of early detection and management.
Conclusion
Vascular dementia is a complex condition that requires a multifaceted approach to management. Understanding the risk factors, symptoms, and treatment options is crucial for patients and their caregivers. With continued research and a focus on lifestyle changes and early intervention, there is hope for better management and improved quality of life for those affected by vascular dementia.
Vascular Dementia: The Most Preventable Type of Dementia
Understanding High Blood Pressure for Vascular Dementia Prevention


You might also like this article: