Understanding Mild Cognitive Impairment
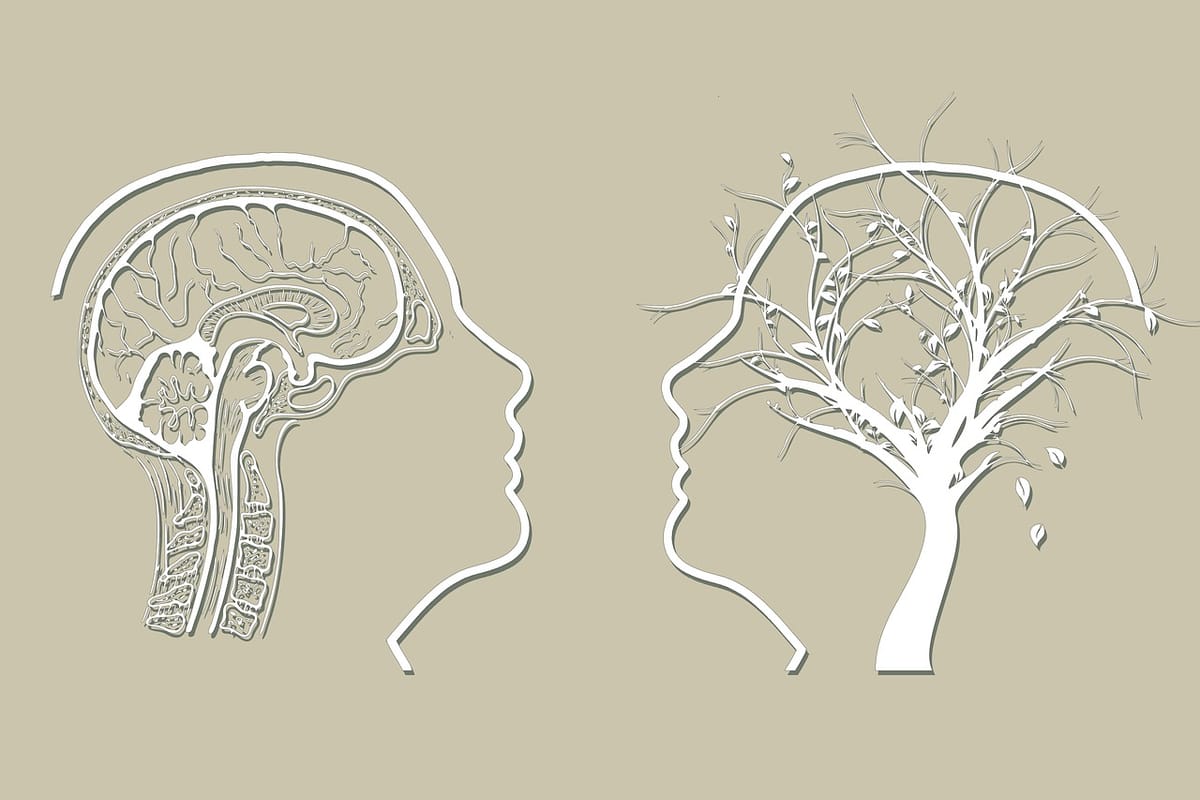
Understanding Mild Cognitive Impairment (MCI) is crucial as it involves noticeable but not disabling memory and thinking problems, potentially leading to dementia. Early recognition and management can slow progression and maintain quality of life in older adults.

What is Mild Cognitive Impairment (MCI)?
Mild cognitive impairment is a medical condition characterized by noticeable changes in cognitive functions, including memory and thinking skills, that are greater than what might be expected from normal aging but not severe enough to interfere significantly with daily life.
MCI and Its Relation to Alzheimer’s Disease
While MCI does not always lead to Alzheimer’s, it can be an early stage of Alzheimer's disease. People with MCI, especially MCI involving memory problems, are at an increased risk of developing Alzheimer’s or another dementia. However, some people with MCI remain stable or even improve over time.
Individuals with MCI may develop dementia, including Alzheimer's disease.
People with MCI are at an increased risk of developing Alzheimer's, particularly early Alzheimer's disease, or other forms of dementia. However, some people with MCI remain stable or even improve over time.
How to Detect Mild Cognitive Impairment Early?
Symptoms and Diagnosis
Mild cognitive impairment (MCI) is a condition marked by a noticeable decline in mental abilities compared to others of the same age. The symptoms of MCI can vary depending on the specific thinking skills affected. Common symptoms include memory loss, language difficulties, and visual/spatial perception problems. Additionally, MCI can cause changes in personality, mood, and behavior, making it a multifaceted condition.
Diagnosing MCI can be challenging, as the symptoms are not as severe as those of Alzheimer’s disease or other forms of dementia. A diagnosis of MCI is made based on a comprehensive evaluation of cognitive and functional abilities. This process often involves a thorough medical history, physical examination, and laboratory tests to rule out other causes of memory problems. Brain imaging, such as MRI or CT scans, may also be used to identify any structural changes in the brain that could be contributing to the symptoms. These diagnostic tools help doctors determine the presence of mild cognitive impairment MCI and differentiate it from normal aging or other medical conditions.
Analyzing Your Experiences
Confusion with Dates and Events: The episodes you describe, such as mixing up dates or planning for events incorrectly, could be related to mild cognitive impairment. These lapses can be considered significant memory problems if they represent a change from your usual ability to manage dates and events. Memory loss is a common symptom of MCI, where individuals experience noticeable cognitive changes without losing the ability to perform daily activities.
Distinguishing from Normal Aging: It’s important to distinguish these memory problems from typical age-related changes. Normal aging might involve occasionally forgetting names or appointments but remembering them later, which differs from the more consistent and disruptive memory lapses seen in MCI.

The Importance of Clinical Evaluation
Given your family history and symptoms, it would be prudent to undergo a clinical evaluation to get mild cognitive impairment diagnosed. This may include:
- Neuropsychological Testing: To assess your memory, thinking skills, and mental status.
- Brain Imaging: MRI or CT scans can help in diagnosing MCI and its progression.
- Blood Tests: To rule out other factors that can cause memory problems, such as vitamin deficiencies or thyroid issues.
Participating in a clinical trial can also be beneficial, as it allows for early intervention and the assessment of new medications like lecanemab and aducanumab.
Risk Factors and Prevention
Family History and Genetics: A family history of Alzheimer’s is one of the strongest risk factors for developing a condition called mild cognitive impairment (MCI) and dementia.
Lifestyle Factors: Regular physical activity, a healthy diet, mental stimulation, and social engagement can help prevent cognitive decline. Avoiding smoking and managing conditions like high blood pressure and diabetes are also important.
Relationship to Alzheimer’s Disease
MCI is often considered a transitional stage between normal cognitive aging and dementia. Research has shown that individuals with MCI are at a higher risk of developing Alzheimer’s disease or a related dementia. In fact, studies indicate that more people with MCI than those without it go on to develop Alzheimer’s disease or another form of dementia. However, it is important to note that not everyone with MCI will develop dementia; in some cases, symptoms may remain stable or even improve over time.
The relationship between MCI and Alzheimer’s disease is complex and not yet fully understood. However, it is clear that MCI is a significant risk factor for developing Alzheimer’s disease. Early diagnosis and intervention are crucial, as they may help in slowing cognitive decline and improving the quality of life for those affected. Ongoing research continues to explore the underlying biology of MCI and its progression to Alzheimer’s disease, aiming to find effective ways to prevent cognitive decline.
Treatment and Management of MCI
While there’s no definitive treatment for MCI, some strategies can help manage symptoms:
- Cognitive Training: Engaging in activities to boost memory and thinking skills. Cognitive training is crucial for maintaining mental abilities in individuals with MCI.
- Medications: Currently, there are no medications approved specifically to treat MCI. However, addressing underlying conditions like depression or sleep problems can be beneficial.
- Supportive Therapies: Counseling and joining support groups can help in dealing with the emotional aspects of MCI.
The Role of Ongoing Research
Research in the field of MCI and Alzheimer’s is rapidly evolving. Clinical trials are continuously exploring new treatment options, potential preventive strategies, and ways to slow cognitive decline.
Taking Proactive Steps
Elaine, it’s commendable that you are paying close attention to these cognitive changes and seeking information. The next step is to consult with healthcare professionals who can provide a comprehensive evaluation and guide you on the best course of action based on your individual circumstances. Remember, early detection and intervention can make a significant difference in managing MCI and improving quality of life.

Preparing for Your Appointment
If you or a loved one is experiencing symptoms of MCI, seeking medical attention promptly is essential. Preparing for your appointment can help you get the most out of your visit. Here are some tips to help you prepare:
- Write down a list of questions: Include questions about your symptoms, medical history, and lifestyle. This will ensure you cover all your concerns during the appointment.
- Keep a record of your symptoms: Note when they started and how they have progressed. This information can provide valuable insights for your doctor.
- Bring a list of medications and supplements: This helps your doctor understand any potential interactions or side effects that could be affecting your cognitive function.
- Bring a friend or family member: Having someone with you can provide support and help you remember what the doctor says.
- Be prepared to discuss your mental function: Share any changes you have noticed in your memory, thinking skills, or problem-solving abilities.
By being well-prepared for your appointment, you can help your doctor make an accurate diagnosis and develop a plan to manage your symptoms and slow cognitive decline. Taking these proactive steps can significantly impact your journey with MCI, ensuring you receive the best possible care and support
Here are more articles on topics you may like: