Transcranial Magnetic Stimulation A Breakthrough Treatment For Depression
Transcranial magnetic stimulation (TMS)? is a procedure that uses magnetic fields to stimulate nerve cells in the brain. the U.S. FDA approves it for conditions like obsessive-compulsive disorder (OCD), migraines, and helping people quit smoking when other treatments haven't worked.

Podcast with Dr Don Dubose MD owner of Future Psych Solutions
Did you know that transcranial magnetic stimulation (TMS) is an amazing procedure that uses magnetic fields to stimulate nerve cells in the brain? It's pretty cool because it can help improve symptoms of major depression without surgery or cutting the skin. The U.S. Food and Drug Administration (FDA) actually approves it for other conditions like obsessive-compulsive disorder (OCD), migraines, and even to help people quit smoking when other treatments haven't worked.
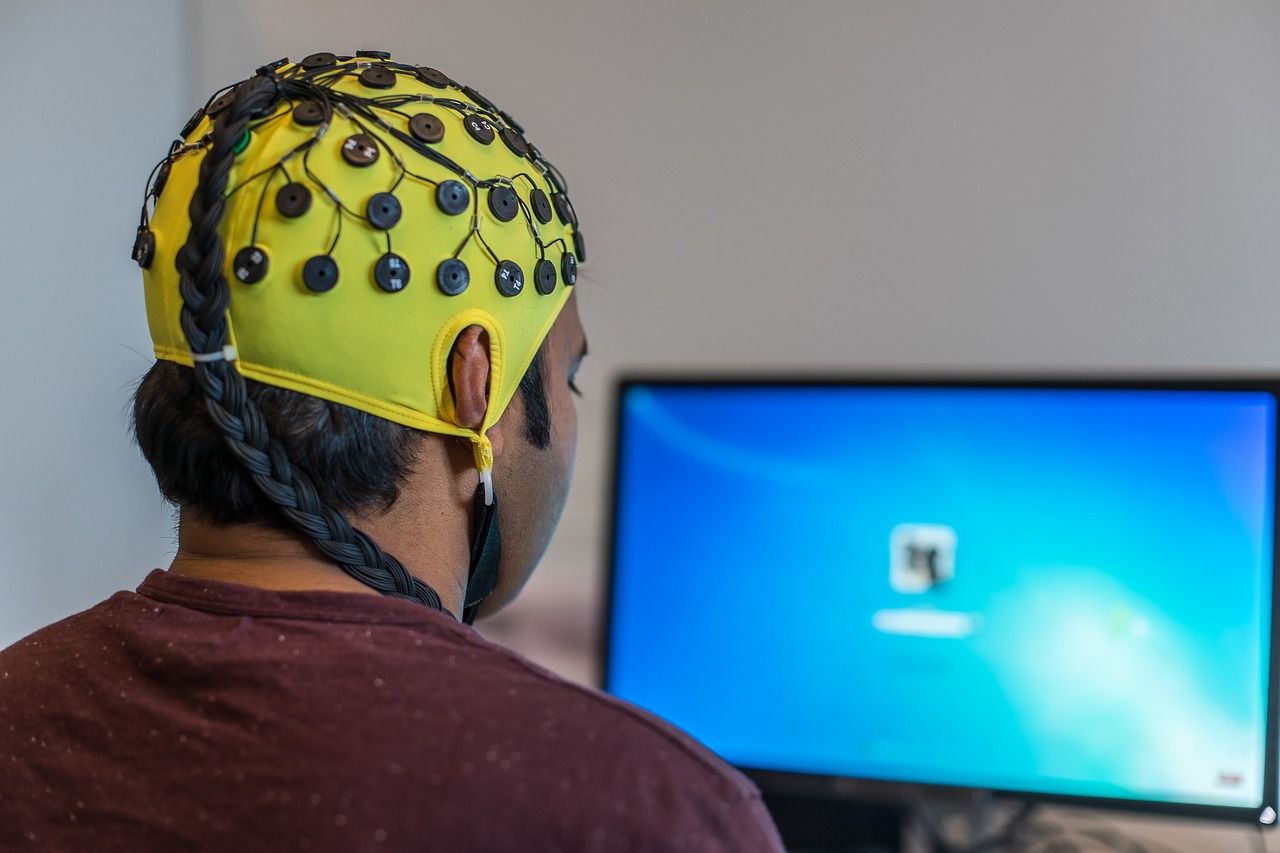
During an TMS session, they place an electromagnetic coil on your scalp to send magnetic pulses that stimulate the regions of your brain involved in mood control. It's believed to activate parts of the brain that have reduced activity during depression, helping to alleviate symptoms and improve mood. How amazing is that?
There's also something called deep transcranial magnetic stimulation (deep TMS) where they use a different type of coil that can reach deeper and wider areas of the brain compared to regular TMS. This one has been FDA-approved for OCD and to help people stop smoking. It's so fascinating how TMS affects the brain and helps with different conditions.
TMS is usually considered when standard treatments like medications and talk therapy don't work for depression. It's also used for other conditions like OCD, migraines, and to help people quit smoking when other treatments haven't been successful.
The best part is that TMS is a noninvasive procedure, unlike other brain stimulation methods. It's a pretty safe option with minimal risks compared to other treatments.
Isn't it fascinating how TMS can improve brain function and make a difference in people's lives? As experts continue to learn more about the most effective ways to perform TMS, the methods may change.
Risk Factors

Let's talk about repetitive TMS, a noninvasive form of brain stimulation. Unlike other methods like vagus nerve or deep brain stimulation, there's no need for surgery or implanting electrodes with TMS. It won't cause seizures or memory loss like electroconvulsive therapy (ECT), and no anesthesia is required either.
Typically, TMS is considered safe and well-tolerated, but it can lead to some side effects.
Common side effects of TMS

Don't worry too much as the side effects are mostly mild to moderate and tend to improve shortly after a session. With more sessions, the side effects become less frequent.
These side effects may include:
Scalp discomfort and pain.
Headaches.
Tingling, spasms, or twitching of facial muscles.
Feeling lightheaded.
Your healthcare provider can always adjust the stimulation level to reduce symptoms, or give you a pain medication prior to the procedure. However, TMS might induce headaches in people who frequently suffer from them, which may require stopping the treatments.
Uncommon side effects of TMS
Serious side effects are quite rare but can include:
Seizures.
Emotional highs, or mania, especially in individuals with bipolar disorder.
Hearing loss if the ears aren't properly protected during treatment.
To determine if TMS has any long-term side effects, further research is needed.
Preparing for TMS
Getting ready for TMS may involve:
A physical examination and possibly other tests or lab work.
A mental health evaluation to discuss your depression.
These evaluations are necessary to ensure that TMS is a safe option for you.
Inform your healthcare provider if:
You're pregnant or planning to be.
You have any metal or implanted medical devices. While rTMS is possible in some cases, the strong magnetic field produced during treatment makes it incompatible with certain devices like:
Aneurysm clips or coils.
Stents.
Implanted stimulators.
Implanted vagus nerve or deep brain stimulators.
Implanted electrical devices, such as pacemakers or medicine pumps.
Electrodes for monitoring brain activity.
Cochlear implants for hearing.
Magnetic implants.
Bullet fragments.
Other metal devices or objects implanted in the body.
You're currently taking any medications, including prescriptions, over-the-counter drugs, herbal supplements, vitamins, or other supplements, along with their respective doses.
You have a history of seizures or a family history of epilepsy.
Remember, it's crucial to have an engaging conversation with your healthcare provider to address any concerns you may have regarding TMS.
How you prepare for your first transcranial magnetic stimulation

Before having TMS, you may need a:
· Physical exam and possibly lab tests or other tests.
· Mental health evaluation to discuss your depression.
These evaluations help make sure that TMS is a safe option for you.
Tell your health care provider if:
· You're pregnant or thinking of becoming pregnant.
· You have metal or implanted medical devices in your body. In some cases, people with metal implants or devices can have TMS. But due to the strong magnetic field produced during TMS, it's not recommended for some people who have these devices:
o Aneurysm clips or coils.
o Stents.
o Implanted stimulators.
o Implanted vagus nerve or deep brain stimulators.
o Implanted electrical devices, such as pacemakers or medicine pumps.
o Electrodes for monitoring brain activity.
o Cochlear implants for hearing.
o Magnetic implants.
o Bullet fragments.
o Other metal devices or objects implanted in their body.
· You're taking medicines, including prescriptions, medicines available without a prescription, herbal supplements, vitamins or other supplements, and the doses.
· You have a history of seizures or a family history of epilepsy.
· You have other mental health conditions, such as issues with alcohol or drugs, bipolar disorder, or psychosis.
· You have brain damage from illness or injury, such as a brain tumor, stroke or traumatic brain injury.
· You have frequent or severe headaches.
· You have any other medical conditions.
· You've had treatment with TMS in the past and whether it was helpful in treating your depression.
How to prepare for your first Transcranial Magnetic Stimulation treatment

Are you ready for your first appointment? Don't worry, repetitive TMS is a non-invasive procedure that doesn't require anesthesia, and you can even go home on your own afterward. However, if you prefer, you can have someone drive you home after the first session to see how you feel.
Before diving into treatment, it's a good idea to check with your health insurance company to find out if rTMS is covered. Most policies cover rTMS for depression, but there may be certain conditions you need to meet, such as trying multiple antidepressants that didn't work. As for using rTMS for OCD or to quit smoking, it's still relatively new, so insurance coverage may not be available yet. However, that could change in the future as its usage becomes more common.
When it comes to the treatment itself, repetitive TMS is typically conducted in a healthcare provider's office or clinic. You'll need multiple sessions for it to be effective, usually five days a week for 4 to 6 weeks. So get ready for a series of appointments that will help you on your journey.
Welcome to your first treatment session! Before we dive in, your health care provider will carefully determine the perfect spot on your head for the magnet and the ideal dose of magnetic energy tailored just for you.
During this appointment, we'll go through a process called "mapping". Here's what you can expect:
You'll be escorted to a cozy treatment room where you can relax in a comfy reclining chair. Don't forget to put on the provided earplugs for the procedure.
An electromagnetic coil will gently be placed against your head. It will create small pulses that might feel like gentle taps on your head and produce a soft clicking sound. Don't worry, there will be short pauses in between.
The coil will be moved around your head, and the magnetic energy will be adjusted until we find the exact spot that causes movement in the fingers or hands on the other side of your body. This will help us determine the optimal placement. Once that's done, we'll begin the next step called "motor threshold". We'll alternate between strong and weak pulses to figure out the precise energy needed to move your fingers or thumb in at least half of the attempts.
Get ready for a unique and interactive experience during your first session!
What happens during your transcranial magnetic stimulation treatment?
Let me walk you through what happens during each treatment session:
First, you'll get comfy in a chair, pop in some earplugs, and have a magnetic coil placed against your head. Just so you know, the treatment spot is different from where the coil makes your fingers or thumb move.
Now, when the machine is switched on, you'll feel and hear some rapid tapping on your scalp. It'll go like tap-tap-tap followed by a pause. This tapping pattern will keep repeating. During the tapping, you might experience some scalp discomfort or even a bit of pain, but don't worry, the pauses will give you a break. And hey, you'll be wide awake and alert throughout the whole procedure.
Depending on the stimulation type used, the treatment will last either 3.5 minutes or 20 minutes. The new "intermittent theta burst stimulation" only takes 3.5 minutes. In the past, the original TMS pattern lasted 37 minutes, but now it's down to 20 minutes for your convenience.
After your TMS treatment

After each treatment, you'll be good to go about your regular activities. There might be a slight headache afterward, but it won't last long. And between treatments, you can continue with work and even drive around as per usual.
If TMS works for you, it can lead to a significant improvement or even complete resolution of your depression symptoms. It may take a few weeks of treatment to start experiencing relief from your symptoms.
As researchers continue to explore and refine TMS techniques, the effectiveness of this treatment may further improve. They are working on determining the optimal number of stimulations needed and identifying the best brain areas to target.
After completing an TMS treatment series for depression, your healthcare provider may recommend ongoing standard care, which could include medication and talk therapy.
At present, it is uncertain whether maintenance TMS sessions can provide continued benefits for your depression. This approach involves continuing treatment even when you are symptom-free, with the hope of preventing the recurrence of symptoms.
If your depression improves with TMS for a period of 2 to 3 months, but you experience symptoms again later on, you have the option to undergo TMS treatment once more. It is worth noting that most insurance companies will cover repeat treatment.





