Managing Sundowner's Syndrome: Strategies and Insights
Dealing with sundowner's syndrome in a loved one with dementia can be exhausting for family caregivers. Learn about the causes and symptoms of sundowner's and tips for managing it through medication, environmental and behavioral approaches.

Sundown syndrome, also known as sundowner's syndrome, is a perplexing condition that primarily affects individuals with dementia or those in the early stages of Alzheimer's disease. As the sun begins to set, these individuals often experience heightened confusion, agitation, and restlessness. Interestingly, some may even display symptoms as early as the afternoon. As the evening progresses, behaviors can escalate, leading to increased negativity, irrationality, confusion, and, in some cases, physical aggression.
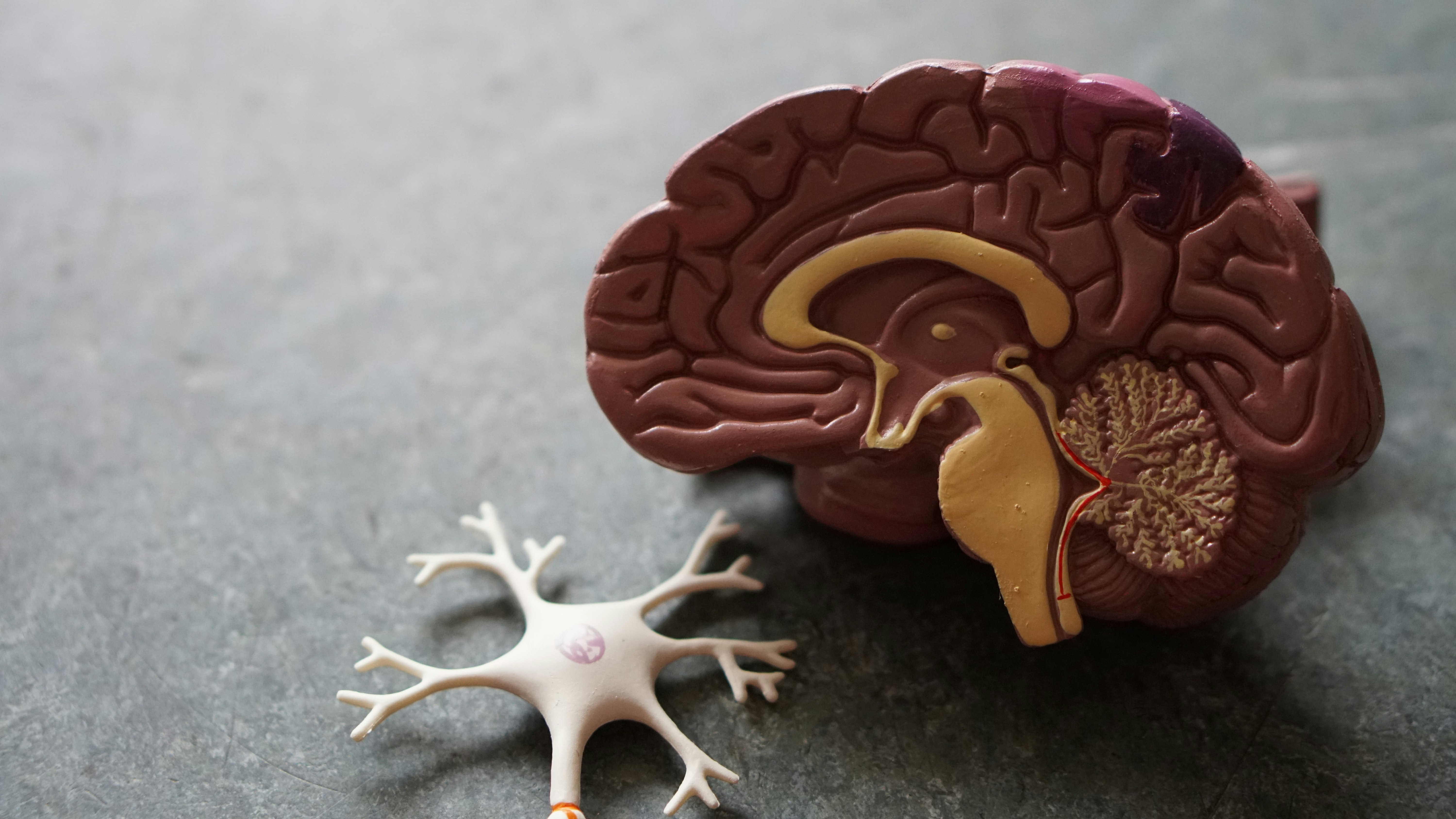
The exact cause of this syndrome remains elusive. Initial theories suggested a malfunction in the brain's internal sleep-wake clock. More contemporary thought centers around the idea that individuals with dementia become fatigued, but instead of transitioning into a restful state, their brains become overactive. This cognitive dissonance, coupled with the cognitive decline they're facing, results in heightened stress and overstimulation, ultimately manifesting as irrational behavior and aggression.
For family caregivers tending to loved ones with sundown syndrome, the experience can be both exasperating and draining. However, there are proactive strategies that caregivers can employ to better manage and cope with this challenging condition. These strategies often encompass a combination of medications, environmental adjustments, and behavioral approaches.
While medical interventions may be suggested by healthcare professionals to alleviate agitation, promote sleep, or address depression, it's crucial for caregivers to integrate behavioral and environmental modifications for more comprehensive results. It's also worth noting that some individuals with dementia might respond paradoxically to medications, where calming medications could exacerbate their agitation and confusion—particularly relevant in cases of Lewy Body dementia.
Enhancing the environment is key, and maintaining a consistent routine is paramount as cognitive function declines. Stability helps counteract the overwhelming nature of changing circumstances and declining abilities. A structured daily routine should incorporate exposure to sunlight or bright light, fostering natural sleep-wake cycles. High-stress tasks should be scheduled earlier in the day, gradually transitioning to less demanding activities as the day progresses.
A brief nap after lunch can be invigorating, but prolonged midday or evening naps should be discouraged. Whenever feasible, engage the individual in an afternoon walk or enjoyable activity to sustain their energy levels. As the afternoon transitions to evening, creating a tranquil atmosphere becomes vital. Drawing curtains or lowering shades can simulate nighttime conditions, helping regulate the sleep-wake cycle. Evening hours should prioritize serenity—minimize noise and distractions, and opt for calming activities like reminiscing with old photographs or discussing cherished childhood memories.
Crafting a consistent bedtime ritual is especially crucial during this stage of dementia. Regardless of the day's events, adhering to a routine at bedtime is vital, especially following the last meal of the day.
The role of a caregiver can be incredibly taxing, particularly when managing someone with sundown syndrome. Prioritizing self-care and rest becomes indispensable for caregivers. This may necessitate seeking assistance from others to effectively support their loved one at home.
In summary, understanding sundown syndrome and implementing these strategies can significantly enhance the quality of life for both individuals with dementia and their devoted caregivers.
More on Sundowner’s Syndrome and How to Handle it
Tips for Dealing with Sundowning and Sleep Disorders in Dementia
You might also like this article: