Parkinson With Dementia
Parkinson's disease is a progressive disorder that can lead to dementia in some cases. Learn about the early signs, risk factors, and treatment options for this condition.

Parkinson’s disease is a progressive disease of the central nervous system. Living with Parkinson's disease can come hand-in-hand with various changes to your physical, mental and emotional wellbeing.
Unfortunately it is possible for patients of the condition to face a decline in thinking abilities if their illness has been present for over 12 months; this deterioration - known as Parkinson disease dementia – involves issues such as cognitive changes, difficulty concentrating, trouble making judgements or planning ahead amongst many other symptoms.
Early signs and symptoms of this movement disorder may have include tremors/shaking hands and body stiffness resulting in postural instability. Communication difficulties progress into slurred speech patterns lacking facial expression. All hallmarks associated with movement difficulties that are common at early stages.
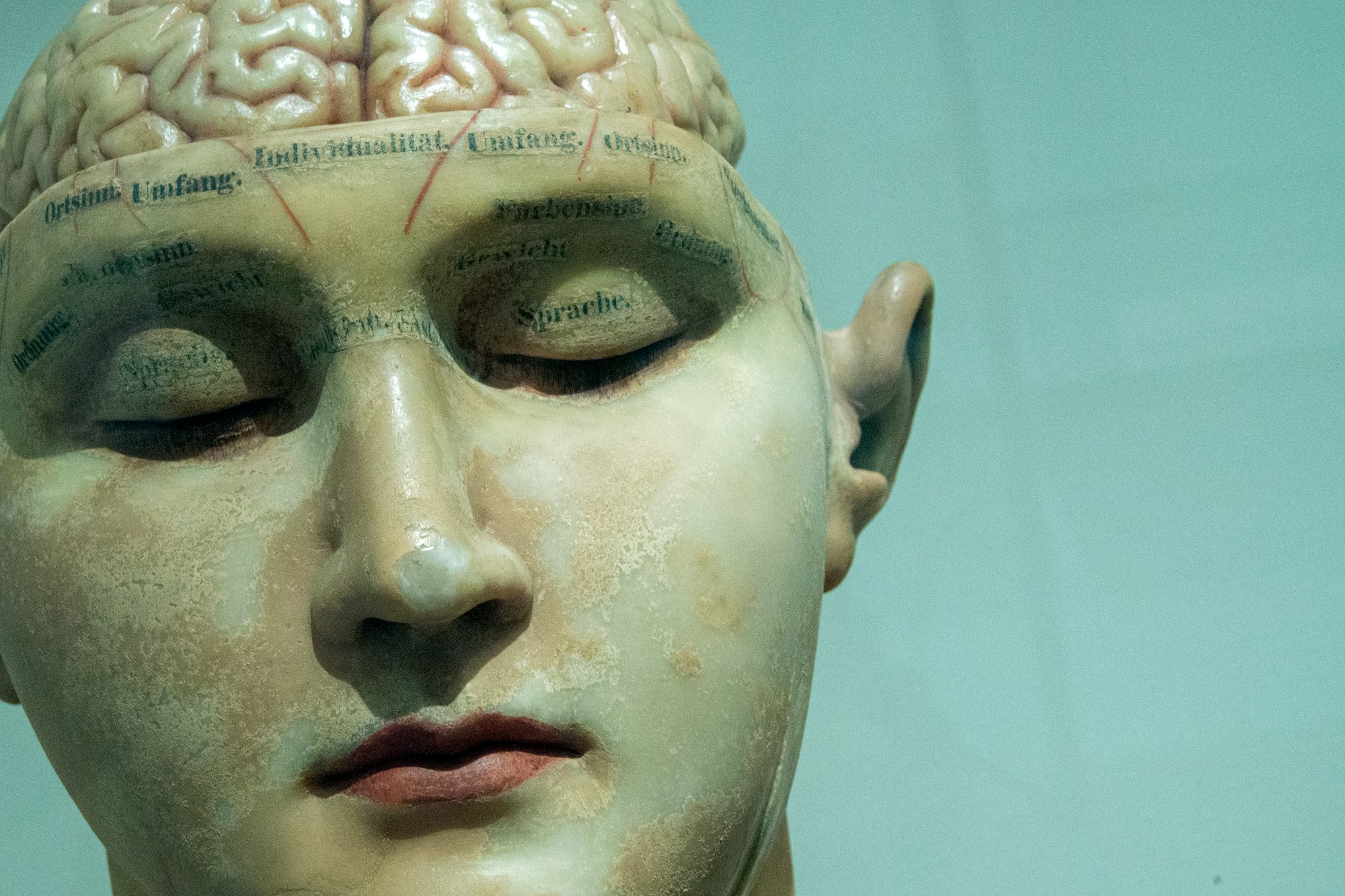
Parkinson's disease and its related Parkinson disease dementia can be traced back to abnormal deposits called Lewy Bodies. Named after Frederick H. Lewy who discovered them while doing research in Alois Alzheimer’s lab at the start of the 20th century. These abnormities are composed mainly of a protein called alpha-synuclein whose purpose is still up not understand today.
Recent research suggests there may be an underlying connection between Dementia with Lewy Body, and Parkinson Disease Dementia which is related to errors in how alpha-synuclein proteins are processed by brain cells. In some cases individuals also have both plaques & tangles associated with Alzheimer's disease; this combination is commonly called mixed dementia.
Causes

Living with Parkinson's for 10 years or more can dramatically increase your risk of developing dementia. Researchers have reported that, on average, it takes about a decade from onset to the development of dementia-related symptoms in patients. Before they develop full-blown disease states like this one, individuals are likely to experience milder cognitive changes labeled as Mild Cognitive Impairment (MCI). While those who had normal cognition when diagnosed may only need five years before MCI appears; every individual is unique and these numbers vary person by person.
If you've been diagnosed with Parkinson’s, there are a few factors that could indicate an increased risk for dementia in the future.
These may include:
Advancing age,
More severe motor symptoms
Mild cognitive impairment
Hallucinations without other signs of dementia
Postural instability gait disturbance (PIGD).
It is essential to be aware of these indicators so preventive measures can be taken early on.
Risk Factors
Several theories that have been formulated using the results of many research studies regarding the cause or causes of Parkinson’s disease include:
- Genetic abnormalities
- Environmental toxins that may attack and damage dopaminergic neurons (carbon monoxide, manganese and some pesticides)
- Oxidative stress enacted by free radicals
- Strong antipsychotic medications designed to relieve symptoms of schizophrenia and psychosis
Doctors specializing in neurodegenerative diseases speculate that Parkinson’s may develop because of a combination of one or more of these factors.
Receiving a correct diagnosis and initiating a treatment plan at the initial onset of Parkinson’s disease is the best way to slow the progression of muscle rigidity and cognitive impairments. In addition, many Parkinson’s patients live semi-independently for many years following a diagnosis but may eventually deteriorate to a point where 24-hour care is necessary.
Parkinson's Disease Dementia

Common symptoms involving the Parkinson disease dementia exhibit varying degrees of difficulty regarding:
- Selective attention
- Abstract thinking
- Planning and reasoning
- Recalling encoded information (riding a bicycle or unlocking a door)
- Impulse control (the patient may develop hypersexuality, crave enormous amounts of food or becoming addicted to gambling)
- Mental health conditions such as, depression, anxiety and apathy
- Excessive daytime sleepiness
- Psychiatric symptoms, such as paranoid ideas and visual hallucinations
Behavioral changes affect Parkinson disease patients more often than cognitive symptoms. Although Parkinson disease dementia can produce delusions and/or hallucinations due to dopaminergic excess in the brain.
What is Dopamine?

Dopamine is one of the brain’s most important neurotransmitters, coordinating muscle control, inhibiting muscle contraction and facilitating the ability to perform smooth, planned movements.
Dopamine is essential for muscle control and the ability to perform smooth, planned movements. Its production takes place in a part of the brain called substantia nigra by dopaminergic neurons which are unique due to their permanent nature - they cannot regenerate when affected with Parkinson's disease leading to cognitive function decline over time.
Muscle contraction is controlled by five dopamine receptors–receptor one and five are stimulatory and two, three, and four are inhibitory. Complementing dopamine is another important brain chemical called acetylcholine (Ach receptors), which also regulates muscle contraction through five cholinergic receptors.
Number one, three and five cholinergic receptors are stimulatory; two and four are inhibitory. When someone suffers from PDD (Parkinson’s disease dementia) and associated and dementia with levy bodies (DLB), it is a deficiency in number two, three and four dopamine receptors rather than too much acetylcholine affecting number one, three and five Ach receptors that causes the disease.
Normal muscle functioning occurs when a balance exists between inhibitory and stimulatory signals regulated by these receptors that exist on the surface of nerve cells. When receptors do not receive enough dopamine, but Ach receptors continue receiving the same amount of acetylcholine, Parkinson’s disease dementia slowly begins to overwhelm the patient. Along with the motor symptoms that eventually leave the affected individual unable to walk or initiate independent movement.
Parkinson' s Disease Dementia versus Lewy Body Dementia

Have you ever wondered how dementia with Lewy bodies and Parkinson's disease dementia differ? While they may sound similar in terms of the symptoms, these two disorders are actually both forms of Lewy body dementia. To gain a better understanding between Parkinson's disease dementia and dementia with levy bodies, it is important to recognize that each has both physical (muscle weakness, rigidity, slowed movement) as well as mental manifestations(impaired executive functioning attention span memory loss). Be sure to know what signs to look for when distinguishing between them.
When degeneration of the brain areas underneath the cerebral cortex occurs as it does in Parkinson’s, this type of dementia is called subcortical dementia. Symptoms of subcortical dementia include most of the signs of Alzheimer’s dementia–memory and speech problems, irrationality, memory problems and depression.
Certain brain structures, such as the basal ganglia, are especially damaged by lewy bodies , which causes severe difficulties with controlling voluntary movements. Huntington’s disease is another example of a neurodegenerative disorder producing subcortical dementia and difficulties regulating muscle control.
There are two sets of symptoms that occur in both Parkinson's Disease Dementia and Dementia with Lewy Bodies:
Both of these are a type of Lewy body dementia and have symptoms that affect the body and the brain. Hallucinations and depression are often present in both types of dementia, as well. Both conditions are often treated by medications typically prescribed for Parkinson's disease, such as carbidopa-levodopa (Sinemet), which may be helpful by improving the ability to move and physically function, as well as
How are Parkinson Disease Dementia and Dementia with Lewy Bodies Different?
That's a good question, because it depends on whom you ask. Some health professionals feel that these are two conditions that are versions of the same condition. In fact, some health professionals use the terms interchangeably. Yet, diagnostic guidelines determine there are some differences.
While both types of dementia share some common characteristics, such as the presence of Lewy bodies in the brain and atrophy of cells that send out acetylcholine neurotransmitters, a unique trait linked more closely to DLB is an accumulation amyloid beta proteins within brain tissue. This singular feature often helps differentiate between these two distinct forms of cognitive changes.
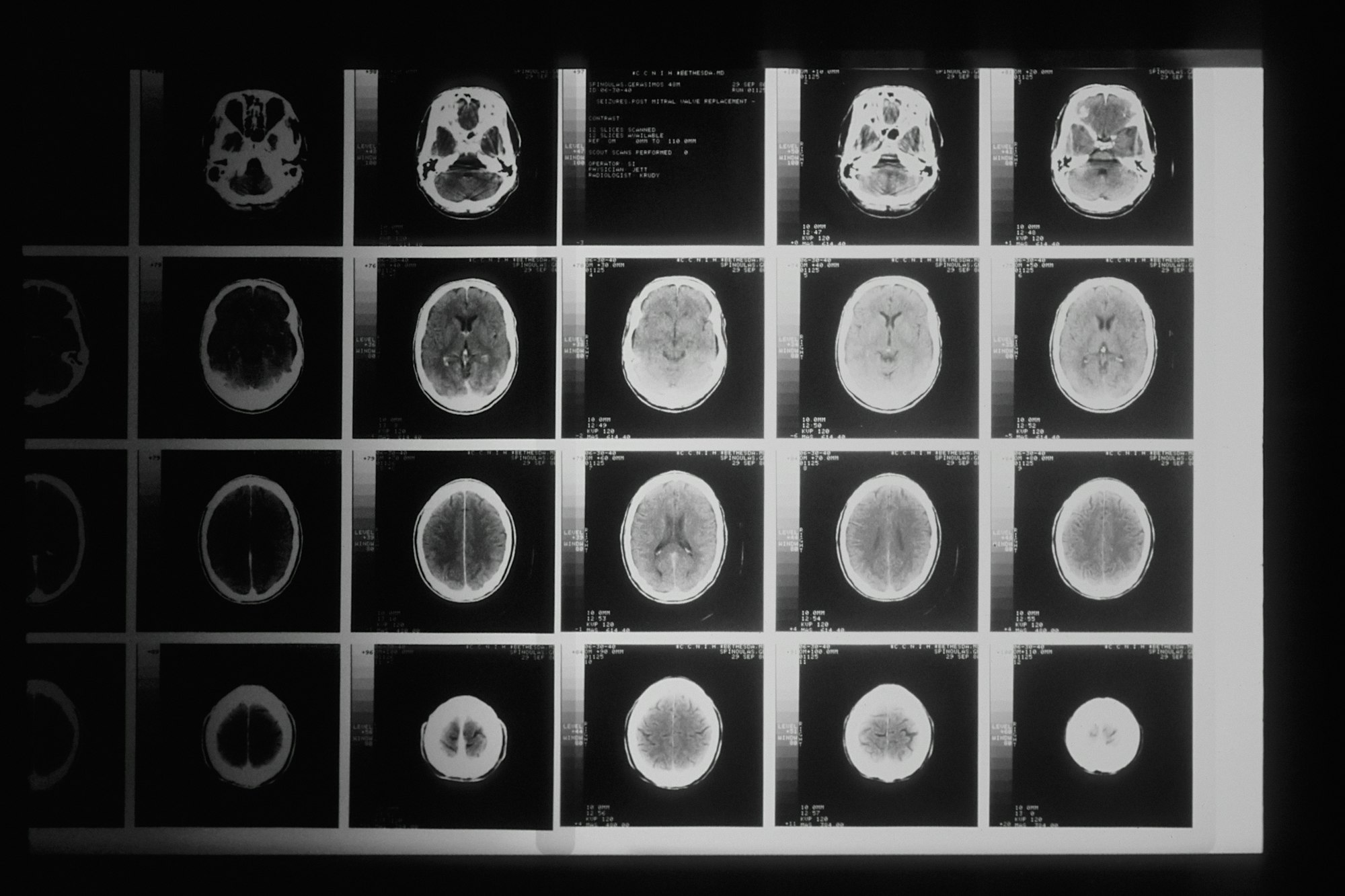
Onset of Symptoms
The biggest difference between Parkinson's disease dementia and Lewy Body dementia is the order of onset of the symptoms. Health professionals usually distinguish between these two disorders by asking which set of symptoms (body or brain) appeared first.
To diagnose Parkinson's disease dementia, the motor and movement symptoms, including rigidity, weakness, and tremors, should be present at least one year before cognitive changes develop.
When diagnosing dementia with Lewy bodies, healthcare professionals look for a tell-tale trifecta - motor symptoms and muscle weakness paired with cognitive decline. If the ]cognitive changes come before the mobility issues or within one year of them occurring, it's likely this type of disease is present.
Cognitive Changes

It is crucial to be aware of the potential for variation in cognitive ability between individuals with dementia. For example, those suffering from Lewy bodies dementia tend to experience more fluctuations compared to Parkinson's disease dementia patients. This information can help family members and caregivers distinguish normal ups and downs versus true mental decline or impairment – allowing them greater insight into the patient’s condition as it progresses over time.
Additionally, this knowledge should also factor into any cognitive testing designed for diagnosis purposes , enabling a more comprehensive overview that takes variations due to illness progression into account.
Sleep Disturbances

If you're noticing odd or disruptive nighttime behaviors in someone close to you, it could be an early sign of Lewy Body dementia. This form of dementia is known for causing REM sleep disorder - where people act out their dreams while sleeping, much more than other types like Parkinson's disease dementia.
Parkinson’s Dementia Medications

Levodopa, or L-dopa, a dopamine agonist may alleviate movement symptoms early stages in the disease. Although L-dopa is usually effective at the onset of Parkinson’s, as the disease progresses, dramatic loss of dopaminergic neurons eventually overrides the ability of the drug to relieve muscle tremors and rigidity.
Moreover, the longer Parkinson’s patients take L-dopa, the better chance that they will develop a disorder called dyskinesia, which makes the patient experience uncontrollable writhing movements.
Patients are sometimes helped by physical therapy, deep brain stimulation or surgery in the most advanced Parkinson’s cases, where medication is no longer effective Other therapies currently being researched are stem cell transplants and gene therapy, but have yet to be implemented successfully in the treatment of Parkinson’s.
Parkinson’s disease is managed with medications called cholinesterase inhibitors. These medications increase the levels of acetylcholine, an important neurotransmitter in the body needed for communication between nerve cells. They are only available with a prescription.
One of these drugs commonly used Excelon patch or capsules containing rivastigmine, the same ingredient contained in the patch. However, only mild to moderate Parkinson disease dementia are treatable with this FDA-approved medication. Severe symptoms require alternative and more aggressive therapies.
What Kind of Health Professional can Diagnoses PDD and LBD?

Primary care providers are an appropriate, first-step resource in the early stages. They will address your concerns if you are experiencing any cognitive, behavioral, or physical changes.
Neurologists generally possess the specialized knowledge necessary to diagnose specific types of dementia or movement disorders. Other health professionals that may or may not be available in your area are: neuropsychiatrists and neuropsychologists. These specialists may require a referral from your primary care provider. Geriatricians, who specialize in treating aging senior, are also familiar with the different types of dementia.
Parkinson's Disease Dementia Symptoms: Similarities and Differences
A Person Centered Approach to Dementia Care
Series on Successful Dementia Home Care Tips
Late Stage Dementia Care: Are Hospitalizations Necessary?
http://www.parkinson.org/parkinson-s-disease.aspx
http://www.alz.org/dementia/parkinsons-disease-symptoms.asp
http://www.lef.org/protocols/neurological/parkinsons_disease_01.htm
http://www.alz.org/dementia/parkinsons-disease-symptoms.asp
http://www.lef.org/protocols/neurological/parkinsons_disease_01.htm
You might also like this article: