Navigating the Journey: Balancing Treatment and Comfort in Cancer Palliative Care (Part 4)
Part 4 of 'Navigating the Journey' delves into balancing aggressive cancer treatment with palliative care. It highlights the importance of symptom management, informed decision-making, and enhancing life quality for patients and families in cancer care

Understanding Palliative Care in the Cancer Context
In the complex and often heart-wrenching journey of cancer treatment, patients and their families face a critical crossroad: the decision between continuing aggressive treatment and transitioning to palliative care. This fourth article in our series, “There is a Time to Treat and a Time to Let Go,” delves into this pivotal phase, underscoring the importance of informed decision-making and the role of palliative care in enhancing the quality of life for cancer patients.
Learn how palliative care supports your family member going through cancer treatment
Integrating Palliative Care in Your Cancer Experience
Palliative care, an often misunderstood aspect of cancer treatment, represents a multidisciplinary approach crucial in the holistic management of cancer. Contrary to common perception, palliative care is not confined to end-of-life scenarios. Instead, it encompasses a broad range of services aimed at providing relief from the myriad symptoms, pain, and psychological stress associated with serious illnesses like cancer. This approach plays a pivotal role in enhancing the quality of life not only for the patient but also for their families.
The scope of palliative care in the context of cancer is expansive. It involves a team of health care professionals, including palliative care specialists, doctors, nurses, social workers, and other therapists. This team works collaboratively with the patient's oncology team to integrate palliative treatment seamlessly with cancer treatments such as chemotherapy, radiation, or surgery. The goal is to offer a more comprehensive, patient-centered care approach that addresses the physical, emotional, spiritual, and practical needs of cancer patients.

Palliative Cancer Treatments Symptom Management
One of the key aspects of cancer palliative care is symptom management. Cancer and its treatments can lead to a wide range of symptoms like pain, fatigue, nausea, loss of appetite, and shortness of breath, significantly impacting the patient's quality of life. A palliative health care team excel in controlling these symptoms, thereby helping patients maintain their strength and carry on with daily activities as much as possible.
Besides physical symptoms, cancer patients often grapple with mental health concerns like anxiety and depression. Palliative care services provide emotional support, helping patients and families navigate these complex feelings. This support extends to spiritual care, recognizing and respecting the spiritual or religious needs of patients, which can be particularly important in coping with a cancer diagnosis.
Supportive Care Helps with Controlling Symptoms
Advanced palliative care and early integration into the cancer treatment process have been shown to improve patients' quality of life and even extend survival in some cases. Research from the National Cancer Institute and various clinical trials supports the early introduction of palliative care as part of standard oncology care. This proactive approach helps in relieving symptoms, managing side effects, and providing emotional and social support right from the diagnosis, through treatment, and beyond.
In the context of advanced cancer palliative care treatments becomes even more crucial. It helps patients understand their treatment options and make informed decisions that align with their goals and values. Advance care planning, a key component of palliative care, involves discussing and documenting patients' preferences for future medical care, thus ensuring that their wishes are respected throughout their cancer journey.
Research shows those that utilize palliative care have improved quality of life.
Furthermore, palliative care can help extend services beyond the hospital setting. Palliative care teams assist in coordinating care across various settings – be it in the hospital, at home, in outpatient clinics, or long-term care facilities. This continuous support helps in addressing employment concerns, financial and legal planning, and ensuring that patients receive comprehensive care wherever they are.
Palliative care in the cancer context is an integral part of the health care system, dedicated to improving the quality of life for cancer patients and their families. By addressing the full spectrum of needs – physical, emotional, spiritual, and practical – and by working closely with the oncology team, palliative care professionals ensure that patients receive personalized, compassionate care that supports their well-being throughout their cancer experience.
The Tough Questions: Treatment Prognosis and Side Effects
Cancer treatments, particularly in advanced stages, come with a spectrum of side effects. It's vital for patients to have clear, honest conversations with their healthcare team about the expected outcomes and potential adverse effects of treatments like chemotherapy. Questions such as the likelihood of cure, life expectancy with and without treatment, and the nature of side effects are fundamental. Understanding these aspects helps patients make choices that align with their values and quality of life goals. At the end of this post I have included a list of questions you may ask regarding treatment and prognosis, questions about advanced planning , and then questions you may want to ask yourself.
Planning Ahead: Facing the Future with Courage and Clarity
When dealing with a cancer diagnosis, particularly at an advanced stage, planning for the future becomes a critical aspect of care. Patients should consider discussing wills, out-of-hospital DNRs (Do Not Resuscitate orders), and appointing a Power of Attorney for health care decisions. Additionally, addressing legal and financial issues, and discussing care preferences with family members are steps that can provide peace of mind and reduce future burdens.
Self-Reflection and Legacy: Beyond Medical Decisions
Cancer journey isn't just about medical treatments; it’s also a time for personal reflection and legacy planning. Patients might ponder over life review, spiritual and psychological support, repairing relationships, and planning for their legacy. This period can be a time of profound personal growth, understanding, and connecting with what truly matters.
Palliative Care Team: A Pillar of Support
A palliative care team, comprising specialists in palliative medicine, nurses, social workers, and other health care professionals, offers comprehensive support. They work collaboratively to relieve symptoms, control pain, and provide emotional and spiritual support. Early integration of palliative care into standard oncology care can lead to better quality of life and even improved survival rates.
End of Life Care: Transitioning with Dignity
As cancer progresses, discussions about hospice care and end-of-life planning become increasingly important. It’s crucial for patients and families to understand when and how to make this transition, ensuring that the patient’s final days are spent with dignity, comfort, and surrounded by loved ones.
In conclusion, navigating the journey of advanced cancer involves balancing curative or life-prolonging treatments with the quality of life considerations. Palliative care, with its holistic approach, plays a pivotal role in this journey, offering support, relief, and guidance through the complexities of treatment and end-of-life decisions. Understanding the options, asking the right questions, and planning ahead can empower patients and their families to make decisions that resonate with their goals, values, and preferences.
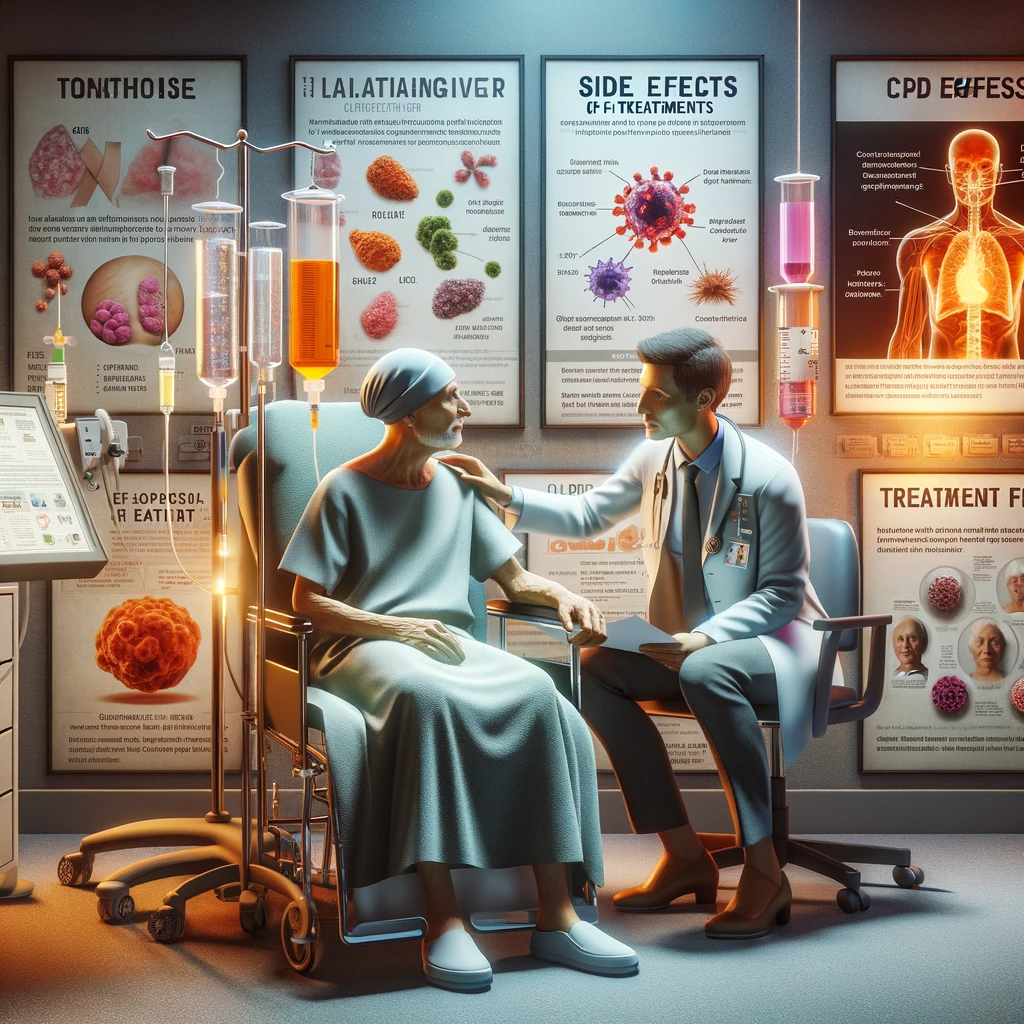
Palliative cancer treatments and side effects of treatments
Palliative cancer treatment side effects can be difficult to endure for many patients. I feel that patients need to be armed with facts and an understanding of their disease.
This will help them to make educated choices about their future care needs.
Many oncologists and cancer treatment teams are often reluctant to bring up-end of life discussions. It is important to know the right questions to ask the professionals…when you are receiving palliative chemotherapy or chemotherapy … that is unlikely to cure cancer, but may extend the length of your life.
Questions Regarding Treatment and Prognosis
- What is my chance of being cured?
- What is the chance that this chemotherapy will slow my cancer? Stay stable? Grow?
- If I start chemotherapy, will it prolong my life? Can you give me a time frame of life expectancy?
- What are the main side effects of the chemotherapy?
- Will I feel better or worse with chemotherapy?
- Are there clinical trials available? What are the benefits? Am I a candidate? What is needed to enroll?
- What are the likely things that will happen to me?
- Will you tell me when hospice or palliative care is appropriate?
- How do you help others make this difficult decision?
- How long to you think I will live with treatment? Without treatment? (this is a time to ask for a range and most likely scenario and when death may be expected)
Questions to ask about Planning Ahead
- Are there things that I should be doing to prepare for my future care needs?
- Should I start preparing my will?
- Is it time to put an out of hospital DNR in place?
- Do I need to put a Power of Attorney for health care in place?
- Are there legal or financial issues that I should be addressing?
- Will you help me talk with my children and family?
Questions You should ask Yourself
- Spiritual and psychological: Who can help me cope?
- Who do I want to
- Legacy and life review: What do I want to pass on to my family to tell them about my life?
- Should I set up a family trust?
- What do I need to do to plan my funeral to make it easier for my family when I am gone?
- What relationships do I want to repair, at this time in my life
Navigating Choices in Cancer Care: Balancing Life Quality and Treatment Goals part 2
Is Palliative Care End of Life Care?
Understanding and Managing Cancer Treatment Side Effects: The Role of Palliative Care
Facing Our Own Mortality: When Life is Not As Long As We Want It To Be
Here's a link to a podcast on Exploring Death and Dying - Dying to Talk
Advanced Planning - How to talk with your health care provider
Embracing Life and Beyond: A Personal Reflection on Death and What Lies Ahead





