Navigating Sundowning Medication and Sleep Disturbances for Better Nighttime Harmony
Explore effective strategies for managing sundowning and sleep disturbances in dementia. Our guide covers medication, behavioral therapies, and environmental adjustments to improve sleep cycles and reduce nighttime agitation.

In the realm of dementia care, one of the most challenging symptoms for both patients and caregivers is sundowning, a term that refers to increased confusion, agitation, and restlessness that typically occurs in the late afternoon and evening. It is also called sundown syndrome. This phenomenon is closely linked with various sleep disturbances, such as a disturbed sleep-wake cycle, difficulty in maintaining sleep (sleep maintenance), and problems with falling asleep (sleep latency). Understanding and addressing these issues is crucial in improving the quality of life for those with dementia and their caregivers.
Understanding Sundowning and Its Impact on Sleep
Sundowning, while not a disease itself, is a symptom commonly seen in Alzheimer’s disease, vascular dementia, Lewy body dementia, and other forms of cognitive impairment. It disrupts the natural sleep-wake cycle (circadian rhythm), leading to symptoms like agitation, confusion, and irritability during the evening or night. This disruption can exacerbate sleep disturbances like sleep fragmentation, where the sleep cycle is interrupted frequently, leading to poor sleep quality.
The exact cause of sundowning is not completely understood but is believed to be related to the deterioration of brain regions that regulate sleep and circadian rhythms. Environmental factors, such as reduced lighting and increased shadows, can also contribute to increased confusion and agitation during these hours.

Behavioral and Psychological Symptoms of Sundowning
Sleep disturbances in dementia patients are a multifaceted issue, often exacerbated by the complex interplay of cognitive decline, behavioral symptoms, and physiological changes. These disturbances, encompassing a range of symptoms like sleep latency, sleep fragmentation, and irregular sleep-wake cycles, are not just symptoms of the condition but also contribute to its progression.
In dementia, especially types like Alzheimer's disease, Lewy body dementia, and vascular dementia, the neurologically compromised brain struggles with maintaining a normal circadian rhythm. This disruption leads to a disturbed sleep-wake cycle, where patients find it difficult to fall asleep (sleep latency) and experience fragmented sleep patterns. Nighttime can become a period of increased activity (nocturnal activity) and agitation, often referred to as sundowning or sundown syndrome.
Sundowning Symptoms
Sundowning, a term used to describe the worsening of neuropsychiatric symptoms such as confusion, anxiety, and agitation in the late afternoon and early evening, significantly impacts the quality of sleep in dementia patients. It is not just a challenge for the patients but also for family caregivers and nursing home staff, who often witness increased agitated behavior and disruptive behavior in patients during these hours.This is the time when agitate nursing home residents show behavioral disturbances.
The treatment of sundowning and associated sleep disturbances in dementia involves both pharmacological and non-pharmacological approaches. Medications, including antipsychotic medications and a selective serotonin reuptake inhibitor (SSRIs), are commonly used. However, these medications come with a risk of adverse effects, especially in older adults and those with severe dementia, making their use a subject of careful consideration and often as a last resort.
Non-pharmacological interventions have gained prominence in managing sundowning behavior. Bright light therapy, for instance, has shown promise in randomized controlled trials for realigning the circadian rhythm and improving sleep quality in dementia patients. Similarly, music therapy, known for its calming effect, can help reduce evening agitation and improve the overall rest-activity rhythm.
Physical exercise, tailored to the capability of the patient, can also play a role in mitigating circadian rhythm disturbances. Regular physical activity, especially in the early part of the day, can help promote better sleep patterns and improve cognitive function.
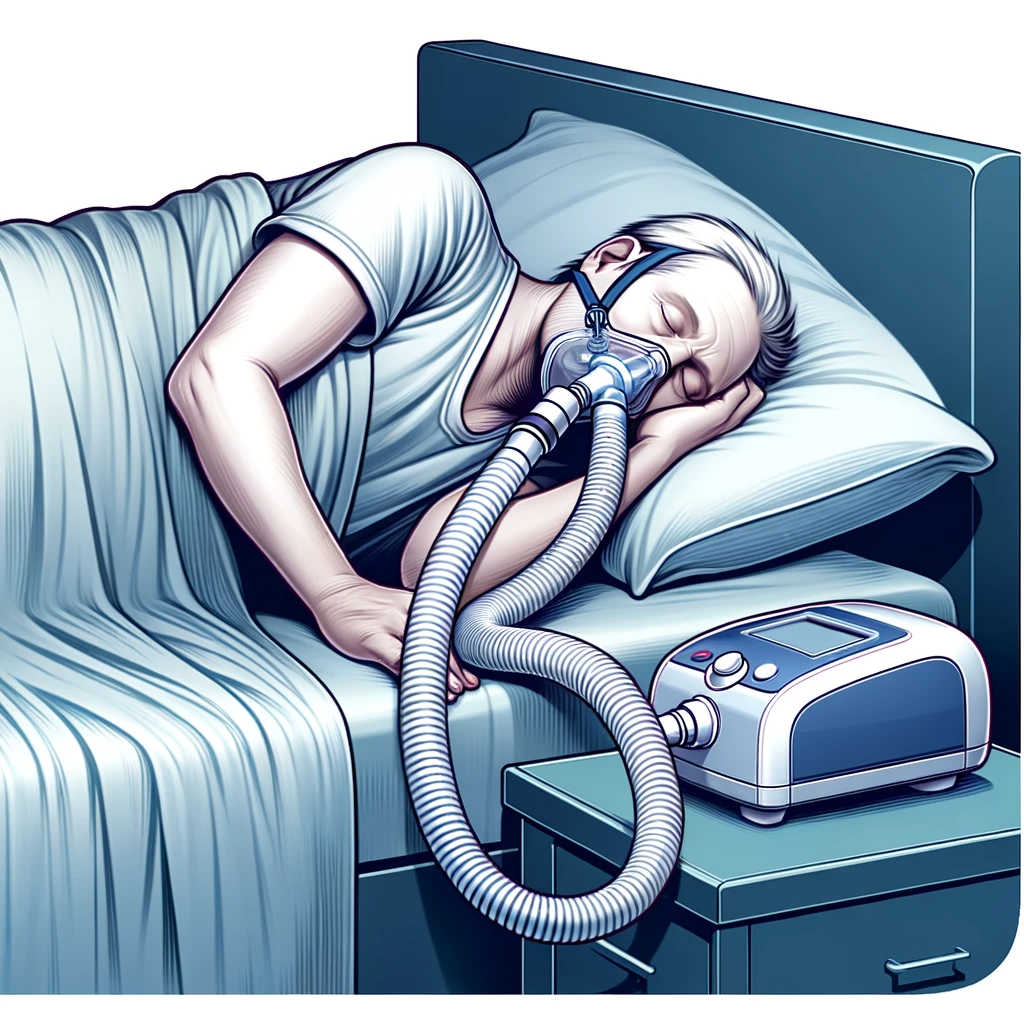
Sleep apnea causes a disturbed sleep wake cycle
Another critical aspect is the management of other sleep-related disorders that often coexist with dementia, such as sleep apnea. This condition, characterized by intermittent stopping of breathing during sleep, can worsen cognitive impairment and sundowning behaviors. Treating sleep apnea and other sleep disorders is therefore an integral part of managing sleep disturbances in dementia.
Environmental factors also play a significant role. Ensuring a comfortable sleeping environment, minimizing noise and light disturbances, and maintaining a consistent sleep schedule can help improve sleep maintenance and reduce the incidence of nocturnal delirium.
In addition to managing the patient’s symptoms, it’s important to address caregiver stress. Family members and institutional caregivers need support and education to understand these behaviors and effectively manage them. Organizations like the Alzheimer's Association provide resources and support for caregivers dealing with these challenges.
In conclusion, managing sleep disturbances in dementia, particularly in relation to sundowning, requires a comprehensive approach. While medications can be necessary, their use must be balanced against the potential for significant negative side effects. Non-pharmacological strategies, including behavioral modifications, environmental adjustments, and therapeutic interventions like light therapy and music therapy, are critical in creating a more harmonious nighttime environment for dementia patients. By addressing these aspects, caregivers can help reduce the burden of sundowning and improve the quality of life for both dementia patients and their caregivers.
Medications and Management Strategies for Sundowning
When it comes to managing sundowning and associated sleep disturbances, a combination of pharmacological and non-pharmacological approaches is often recommended. Medications may be prescribed to help manage the symptoms of sundowning, but their use should be approached with caution due to the potential side effects and interactions with other drugs commonly used by elderly patients.
Antipsychotics:
These medications can be effective in reducing agitation and confusion but are associated with significant risks, especially in older adults. The use of antipsychotics in dementia patients is a subject of ongoing debate and should be considered carefully.
Melatonin and Sleep Aids:
Melatonin supplements can be helpful in regulating the sleep-wake cycle. Other sleep aids might be prescribed to help with sleep latency and maintenance, but their long-term use is generally not recommended due to potential dependence and other adverse effects.
Non-Pharmacological Approaches:
Techniques like maintaining a regular sleep schedule, ensuring adequate exposure to daylight, and providing a calm and comfortable sleeping environment are crucial. Behavioral interventions, such as relaxation techniques and cognitive-behavioral therapy, can also be effective.
Managing Environmental Factors:
Reducing noise and light disturbances during the night, using night lights to reduce shadows and confusion, and ensuring a comfortable room temperature can help in reducing the symptoms of sundowning.
The Importance of Caregiver Support and Education
Caregivers play a crucial role in managing sundowning and sleep disturbances in dementia patients. Education about the nature of these symptoms, effective communication strategies, and coping mechanisms for stress is vital. Support groups and resources provided by organizations like the Alzheimer’s Association can be invaluable in this regard.
Conclusion
Sundowning and related sleep disturbances pose significant challenges in the care of dementia patients. While there is no one-size-fits-all solution, a combination of appropriate medication use and non-pharmacological strategies can greatly aid in managing these symptoms. It is essential to work closely with healthcare professionals to tailor a plan that suits the individual needs of each patient and to provide ongoing support and education for caregivers. With the right approach, it is possible to improve sleep quality and overall well-being for those affected by dementia and their caregivers.
Understanding dementia behaviors: Tips and strategies





