Comprehensive Guide to Managing and Treating Varicose Vein: From Prevention to Advanced Care
Explore our in-depth guide on managing and treating varicose veins, covering everything from prevention techniques to advanced medical treatments. Learn about lifestyle changes, compression therapy, and innovative procedures to alleviate symptoms and improve vein health.

Varicose vein, a common vascular issue, affect various body parts. However, legs often bear the brunt of this condition, making them prime territory for developing varicose veins. In this article, we delve into the unique dynamics contributing to this phenomenon. We will explore the causes and prevention strategies of varicose veins, specifically focusing on the lower extremities.
What Causes Varicose Veins?
Varicose veins, those twisted, enlarged veins most commonly appearing in the legs, and deep veins are not just a cosmetic concern but can also cause discomfort and lead to more serious health issues. The treatment for varicose veins and spider veins aims to relieve symptoms, prevent complications, and improve appearance. Understanding the various options available for managing and treating these vein issues is essential for those affected.
Varicose veins may develop due to weak or damaged valves in the veins that struggle to maintain the direction of blood flow back to the heart. This malfunction can cause blood to pool in the veins, leading to the swollen, bulging appearance characteristic of varicose veins. Factors such as family history, obesity, standing or sitting for long periods, and pregnancy increase the risk of developing varicose veins.

How to treat varicose veins?
Initial treatment for varicose vein often includes lifestyle changes and self-care measures, such as wearing compression stockings to improve blood flow and reduce pain. Compression garments apply gentle pressure on the legs, helping veins and muscle move blood more efficiently. Maintaining a healthy weight, exercising regularly, and avoiding long periods of sitting or standing can also help manage symptoms and prevent new varicose veins from forming.
For those with severe varicose veins or who experience complications like skin sores, blood clots, or deep vein thrombosis, more advanced treatments may be necessary. Medical procedures for removing or closing varicose veins include sclerotherapy, where a solution is injected into the affected vein to scar and close it, and laser therapy, which uses light energy to seal off affected veins. Larger varicose veins might require surgical interventions, such as vein stripping or vein surgery, to remove or tie off the damaged vein. Newer techniques, such as radiofrequency energy or laser therapy, offer minimally invasive options to treat the affected veins by collapsing and sealing them shut, improving blood flow and alleviating symptoms without the need for significant recovery time.
Did you know you can prevent varicose veins?
Preventing varicose veins, especially for those with a family history or other risk factors small varicose veins, involves managing blood pressure, avoiding high heels and tight hosiery, elevating the legs when possible, and staying active to encourage good blood circulation. If you are a person that stands or sites for long periods of time, you should consider wearing compression stocking. Regular check-ups with a healthcare professional can help diagnose varicose veins early and develop an effective treatment plan tailored to the individual's needs.
While varicose and spider veins can be a source of discomfort and concern for many, various treatment options ranging from conservative self-care to advanced medical procedures can effectively manage symptoms, improve aesthetics, and prevent further vein complications. Adopting healthy lifestyle habits and consulting with a healthcare provider for a personalized treatment approach are crucial steps in addressing this common vascular condition.

Venous Insufficiency: How Veins Work
Understanding the normal functioning of veins is crucial to grasp the causes of varicose veins. Veins play a pivotal role in the circulatory system. They are responsible for carrying blood back to the heart. However, when veins encounter difficulties in this process, a condition known as venous insufficiency can develop. For people already dealing with a vein condition, seeking professional help becomes crucial. A Vein clinic in Orlando can offer tailored solutions that are minimally invasive.
The Role of Inflammation: A Contributing Factor
Inflammation is a key player in the anatomy of varicose veins. Chronic inflammation can further compromise vein walls. It also contributes to the development of conditions like superficial thrombophlebitis. This condition occurs when veins near the skin surface become inflamed, causing severe pain.
Factors Contributing to Varicose Veins: Beyond Genetics
Genetics can predispose you to develop varicose veins too. However, several other factors play a significant role, including:
- Prolonged periods of standing or sitting
- Obesity
- Hormonal changes during pregnancy or menopause
Symptoms of Varicose Veins: Beyond Aesthetics
Recognizing the anatomy of varicose veins goes beyond their visible appearance.
Common symptoms include:
- Aching or cramping in the legs
- Heaviness and swelling
- Skin changes
Understanding these symptoms is crucial for early intervention of varicose veins.

The Anatomy of Varicose Veins
Varicose veins, with their twisted veins and bulging appearance, represent a departure from the norm in the circulatory system. It's essential to grasp the structural changes in their anatomy to understand varicose veins.
Differences Between Healthy and Varicose Veins: A Visual Contrast
Healthy veins maintain a smooth, cylindrical shape with valves that ensure efficient blood flow back to the heart. In contrast, varicose veins exhibit a distorted, tortuous appearance. The structural differences lie in the weakening of vein walls. The malfunctioning of valves leads to the accumulation of blood, swollen veins, and the characteristic bulging.
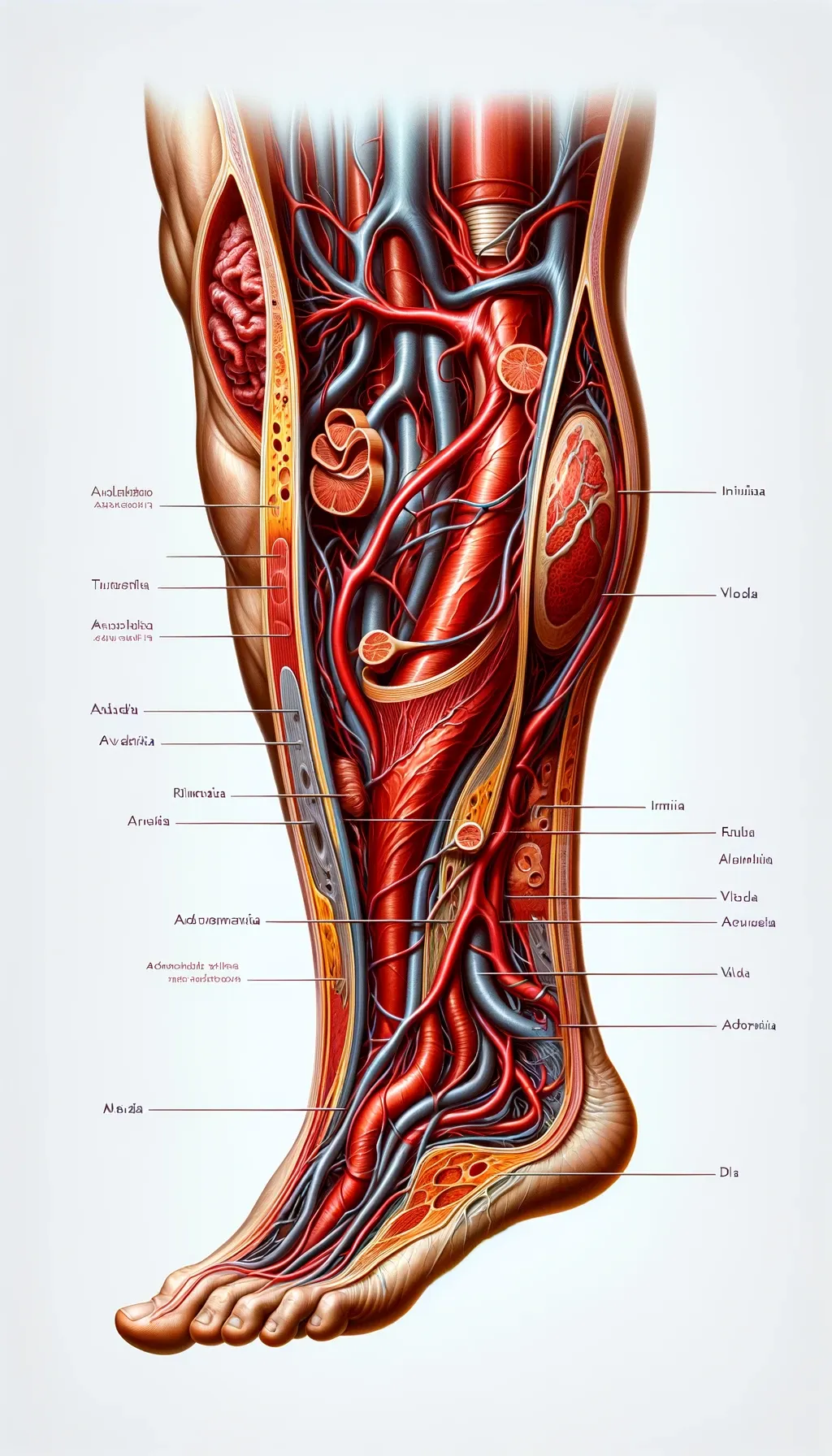
Venous Insufficiency: Weakening of Vein Walls
One of the primary contributors to the anatomy of varicose veins is venous insufficiency. The weakening of vein walls sets the stage for the development of varicose veins. As veins weaken and lose elasticity, they struggle to maintain normal shape and function.
Valve Malfunction: The Culprit Behind Blood Pooling
In healthy veins, valves act as gatekeepers, allowing blood to flow only in one direction—towards the heart. Varicose veins, however, frequently feature malfunctioning valves. This allows blood to pool within the veins—the additional pressure causes the veins to bulge and stretch.
Understanding Gravity's Impact on Circulation
Gravity, that ever-present force keeping us grounded, also exerts a significant influence on our circulatory system. This influence is particularly notable in the veins in our legs. Let's delve into the intricate relationship between gravity and vein health.
The Constant Battle: Blood Circulation Against Gravity
As blood circulates through our bodies, it faces the constant challenge of defying gravity, especially in the lower extremities. Veins are tasked with the responsibility of carrying blood back to the heart. They work against the downward pull of gravity. This constant battle can take a toll on the veins, particularly those in the legs, which are furthest from the heart.
Gravity's Influence in Upright Positions
The effect of gravity on vein health is more pronounced in the upright position. When we sit or stand for a prolonged time, the pressure on the veins in the legs increases.
This increased pressure results from the need to work against gravity. It can cause a gradual weakening of both the vein walls and valves
Wearing Down Veins: The Role of Gravity in Elasticity Loss
Vein walls, like any other tissue in the body, are subject to wear and tear. However, in the case of leg veins, the added challenge of gravity exacerbates this process. Over time, this can result in the loss of elasticity in the veins. This makes the veins more susceptible to dilation and varicosity.
Valve Compromise: The Impact of Gravity on Blood Flow
Moreover, the valves within the veins, responsible for ensuring one-way blood flow back to the heart, can become compromised due to the constant battle with gravity. When these valves fail to function optimally, blood can pool in the veins. This causes them to swell and become visibly distorted – the hallmark of varicose veins.

Lifestyle Choices Amplifying Gravity's Effect
External factors don't solely determine the impact of gravity on vein health. Individual lifestyle choices, such as prolonged periods of inactivity, can exacerbate the veins' gravitational challenge. This is particularly relevant in professions that involve long hours on one's feet or behind a desk.
Proactive Measures Against Gravity's Impact
Understanding the role of gravity in vein health is the first step in developing preventive measures against varicose veins. Simple lifestyle adjustments like the following can help reduce the risk of varicose veins:
1. Taking breaks to walk or stretch during long periods of sitting. This can ease the gravitational stress on leg veins and improve blood flow.
2. Regular exercise, especially activities that promote leg muscle strength. This can enhance blood circulation and provide valuable support to the veins.
Conclusion
Gravity's grasp on our circulatory system, particularly in the legs, highlights the vulnerability of veins to varicose conditions. Addressing varicose veins requires a holistic approach that prioritizes overall well-being. Seek professional advice for personalized guidance on managing varicose veins, ensuring a healthier and more comfortable life.



